Журнал «Здоровье ребенка» 3 (54) 2014
Вернуться к номеру
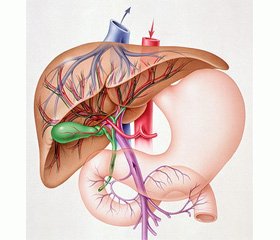
Functional status and metabolic disorders of liver in children with nonalcoholic fatty liver disease and obesity
Авторы: T.O. Kryuchko, O.A. Pylypenko, I.M. Nesina - Higher State Educational Establishment of Ukraine “Ukrainian Medical Stomatological Academy”, Poltava, Ukraine,
Рубрики: Педиатрия/Неонатология
Разделы: Клинические исследования
Версия для печати
metabolic syndrome, nonalcoholic fatty liver disease, children
Currently, the risk factors incorporated in MS are widespread and their prevalence upsurges rapidly due to the increased number of people with obesity. Thus, the incidence of metabolic syndrome in adolescents and young adults has increased as 1.5 times over the past 60 years, and the presence of excessive body weight in children in developed countries is 14 %. The status of the digestive system and its role in the development of metabolic syndrome is currently poorly understood. To date, more and more researchers pay attention to the close relationship between obesity, insulin resistance associated with it, hypertension and dyslipidemia and the development of nonalcoholic fatty liver disease (NAFLD) not only among adults but also in pediatric populations.
The aim of our research was to study the functional status of liver, the disorders of carbohydrate and lipid metabolisms in children diagnosed with NAFLD and exogenously-constitutional obesity (ECO).
Materials and methods. 67 children aged from 7 to 17 have been examined. The main group (n = 34) contained children who were diagnosed with NAFLD; the comparison group (n = 33) consisted of patients with diagnosed obesity without functional disorders of liver; the control group included healthy children (n = 10). All children underwent comprehensive examination which included the collection of anamnestic data, anthropometry and general clinical analyzes. In all patients fasting blood glucose concentration (FBGC) and the level of immunoreactive insulin (IRI) were measured; HOMA and Caro insulin resistance indexes were calculate; the studies of blood lipids were performed with determination of total cholesterol (TCH), triglycerides (TG), cholesterol of high-density lipoproteins (HDL cholesterol), cholesterol of low-density lipoproteins (LDL cholesterol) and cholesterol of very low density lipoproteins (VLDL cholesterol) with account of atherogenic factor.
Results and discussion. The complaints of examined children were noted for their polymorphous nature and, in most cases, they were associated with concomitant diseases of gastrointestinal tract. Almost 53 % of patients in both groups complained of recurrent epigastric pain; 15 % of patients signalized pain in the gastroduodenal region; 42 % of children complained of nausea; recurrent heartburn disturbed 31 % of patients. Probable differences were detected only in complaints of pain in the right upper quadrant (p = 0.00), bloating (p = 0.007), tendency to constipation and stool dilution (p = 0.009), headache, and increased fatigue (p = 0.036) which disturbed children with diagnosed NAFLD more often. The level of total protein and total bilirubin had no significant differences. The fibrinogen level was significantly higher in the group of children with NAFLD as compared with children with ECO (3,27 ± 0,15 and 2,88 ± 0,06 – respectively, p < 0.05), and prothrombin index values tended to decrease in children with NAFLD. The increase of enzimemia was not observed in all children with fatty hepatosis, alanine aminotransferase increase in (ALT) above the physiological norm was observed in 38 % of children; increase of aspartate aminotransferase (AST) was observed in 18 % and increase of gamma-glutamyl transpeptidase (GGT) above the allowable values was observed only in 2 patients (6%). Values of IRI were significantly higher in patients with NAFLD than in children diagnosed with obesity (20,07 ± 1,36 and 12,7 ± 0,75 – respectively, p ≤ 0,01). HOMA insulin resistance index was almost twice as high in children with NAFLD as compared with those with ECO (4,04 ± 0,27 and 2,33 ± 0,15 – respectively, p < 0.01). Index Caro < 0,3 was marked in almost 59 % of patients with fatty degeneration of liver. During examination of blood lipids it was revealed that the group of children with NAFLD, unlike patients with ECO, revealed the highest concentration of serum triglycerides (1,54 ± 0,01 vs 0,98 ± 0,05 mmol / l –respectively, p < 0.01) and lower HDL level (1,03 ± 0,04 mmol / l).
Conclusions. The course of nonalcoholic fatty liver disease in children in most cases is symptomless. Structural and functional changes in liver by nonalcoholic fatty liver disease can cause pronounced metabolic effects in the form of hyperglycemia, hyperinsulinism, insulin resistance with the formation of atherogenic dyslipidemia already in childhood. In order to prevent the development of nonalcoholic fatty liver disease, all children with obesity are recommended to undergo the regular checkups of the structural and functional status of liver, to control the glycemic level and examine the blood lipids.
1. Synytsyn P.A. Metabolichnyy syndrom v ditey ta pidlitkiv. Kliniko-henetychni paraleli: avtoref. dys. na zdobuttya nauk. stupenya kand. med. nauk: spets. 14.01.10 «Pediatriya»/ P.A. Synytsyn.- M., 2009.- 27 s.
2. Serheev V. P. Metabolycheskyy syndrom: prychynы, lechenye y profylaktyka. / Serheev V.P. // Vrach. - 2009.- № 2. - S.36-41
3. Kaydashev Y. P. Эvolyutsyya ponyatyya «metabolycheskyy syndrom» y eho sovremennoe znachenye. / Y.P. Kaydashev // Ukraynskyy medychnyy chasopys. Aktual'ni pytannya klinichnoyi praktyky. -2012. - №2 (88) III – IV.
4. Vos M.B., Welsh J. Childhood obesity: update on predisposing fatstors and prevention strategies. / Vos M.B., Welsh J. // Tsurr. Gastroenterol. Rep. - 2010. - № 12(4). - P. 280-287.
5. Aver'yanov A.P. Ozhyrenye u detey y podrostkov: klynyko-metabolycheskye osobennosty, lechenye, prohnoz y profylaktyka oslozhnenyy./ Aver'yanov A.P.// Mezhdunar. эndokryn. zhurnal. -2009. -№ 4(22). - S. 85¬91.
6. Zimmet P., Alberti G. The metabolits syndrome in children and adolestsents./ Zimmet P., Alberti G. // Lantset.- 2007. 369: 2059–2961.
7. Balыkova L. A. Soldatov O. M. Metabolycheskyy syndrom u detey y podrostkov./ Balыkova L. A. Soldatov O. M. // Pedyatryya.- 2010.- T. 89. № 3. S. 127–134.
8. N.B. Zelins'ka. Metabolichnyy syndrom u ditey./ N.B. Zelins'ka.//Zdorov´ya Ukrayiny.- 2013.-№ 3.-s.48-51.
9. Lazebnyk L. B., Zvenyhorodskaya L. A. Metabolycheskyy syndrom y orhanы pyshchevarenyya. / Lazebnyk L. B., Zvenyhorodskaya L. A. // M., 2009.- 177 s.
10. Bokova T. A., Ursova N. Y. Patolohyya hepatobylyarnoy systemы u detey y podrostkov s ozhyrenyem y metabolycheskym syndromom./ Bokova T. A., Ursova N. Y.// Vrach.- 2011.- № 1. S. 56–58.
11. Skrypnyk Y. N. Yzbыtochnыy ves kak osnova NASH y aktual'naya medyko-sotsyal'naya problema / Y. N. Skrыpnyk // Zdorov"ya Ukrayiny. – 2009. – № 20 (225). – S.6-10.
12. Babak O.Ya. Prychyny ta metabolichni naslidky zhyrovoyi khvoroby pechinky./ O.Ya. Babak //Suchasna hastroenterolohiya.-2010.-№4 (54).- S.8-16.
13. Chernyavs'kyy V.V. Zhyrova khvoroba pechinky yak intehral'na problema vnutrishn'oyi medytsyny /V.V. Chernyavs'kyy // Novyny medytsyny ta farmatsiyi.- 2011.- №4(354). - S.64-67.
14. Stefan N., Kantartzis K., Haring H. Tsauses and Metabolits Tsonsequentses of Fatty Liver./ Stefan N., Kantartzis K., Haring H. // Endotsrine Reviews. -2008. - № 29. - R. 939-960.
15. Bagry H. S. Metabolits syndrome and insulin resistantse / H.S. Bagry, S. Raghavendram, F. Tsarli // An-esthesiology.- 2008. - Vol. 108(3). - P. 506–523.
16. Lamt K.T. Mechanisms of the free fatty atsid-indutsed intsrease in hepatits glutsose produtstion / K.T. Lamt // Am. J.Physiol. Endotsrinol. Metab.- 2003.-Vol.284.- P.863-873.
17.Vasyukova O.V. Ynsulynorezystentnost' pry ozhyrenyy u detey: spornost' otsenky / O.V. Vasyukova, A.V. Vytebskaya // Problemы эndokrynolohyy. – M., 2009. – T. 55, №3. – S. 8–13.
18. A.E. Abaturov. Osobennosty metabolycheskoho syndroma u detey./ A.E. Abaturov.// Dytyachyy likar.-2011.- №4.- s. 54-61.
19. Byelousov Yu.V. Zhyrovyy hepatoz u ditey: definitsiya ta diahnoz / Yu.V. Byelousov, E.N. Babadzhanyan //Suchasna pediatriya.- 2010.- №5(33). -S.107-109.
20. Pylypenko O.A. Kharakterystyka porushen' vuhlevodnoho obminu v ditey z nealkohol'noyu zhyrovoyu khvoroboyu pechinky. / Pylypenko O.A. // Aktual'ni problemy suchasnoyi medytsyny. Visnyk Ukrayins'koyi medychnoyi stomatolohichnoyi akademiyi.- 2013.-Tom 13.- №2 (42). - s. 141-145.