Журнал "Гастроэнтерология" Том 53, №1, 2019
Вернуться к номеру
Вікові i гендерні особливості циркулюючих імунних комплексів та ліпідного метаболізму при запальних захворюваннях кишечника
Авторы: M.V. Stoikevych, I.A. Klenina, O.M. Tatarchuk, V.A. Karachinova, N.S. Fedorova
SІ “Institute of Gastroenterology of the National Academy of Medical Sciences of Ukraine”, Dnipro, Ukraine
Рубрики: Гастроэнтерология
Разделы: Клинические исследования
Версия для печати
Мета: оцінити рівень циркулюючих імунних комплексів (ЦІК) і стану ліпідного обміну в пацієнтів iз віковими та гендерними особливостями перебігу запальних захворювань кишечника (ЗЗК). Матеріали та методи. Проведено обстеження 80 пацієнтів iз ЗЗК: 53 iз неспецифічним виразковим колітом (НВК) та 27 iз хворобою Крона (ХК). Вони були розділені на дві групи залежно від статі: 40 чоловіків та 40 жінок. Крім того, усі хворі були поділені на групи залежно від віку: молодi (45 осiб — 28 iз НВК та 17 iз ХК); середнього віку (15 пацієнтів — 10 iз НВК та 5 iз ХК); похилого віку (20 осiб — 15 iз НВК та 5 iз ХК). Контрольну групу становили 20 практично здорових осіб. У сироватці крові визначали рівень ЦІК, загального холестерину, тригліцеридів, холестерину ліпопротеїнів високої, низької та дуже низької щільності (ЛПДНЩ), коефіцієнт атерогенності. Результати. Рівень ЦІК у сироватці крові вірогiдно перевищував норму в жінок iз ЗЗК — у 1,57 раза (р < 0,05), що можна розглядати як показник інтенсивності запалення, залучення імунної системи до патологічного процесу. У жінок iз НВК рівень ЦІК вірогiдно підвищений — у 1,62 раза (р < 0,05) порівняно з контрольною групою. При ЗЗК уміст ЦІК залежав від віку хворих, він був вірогідно підвищений — у 1,5 раза (р < 0,05) та 1,4 раза (р < 0,05) у пацієнтів середнього та похилого віку відповідно порівняно з молодими хворими. Встановлено кореляцію між рівнем ЦІК та віком (r = +0,552; р = 0,025). Виявлено порушення ліпідного обміну в жінок iз НВК, що виражалося в зниженні вмісту тригліцеридів у сироватці крові в 1,7 разa (р < 0,001), а у чоловіків iз ХК відбувалося зменшення цього показника в 1,5 разa (р < 0,05) порівняно з контрольною групою. У жінок iз НВК вірогідно знижувався рівень ЛПДНЩ в сироватці крові — у 2 рази (р < 0,05), а в чоловіків iз ХК — у 1,8 разa (р < 0,05) порівняно з контрольною групою. Визначено вірогідне зниження вмісту тригліцеридів — у 1,5 разa (р < 0,05) та в 1,6 разa (р < 0,05) у молодих пацієнтів iз НВК та ХК відповідно та в 1,6 разa (р < 0,05) у пацієнтів середнього віку з ХК. Паралельно спостерігалася виражена тенденція до зменшення вмісту холестерину у всіх молодих пацієнтів iз ЗЗК. Визначено вірогідне зниження коефіцієнта атерогенності в молодих хворих. Висновки. Проведені дослідження дозволили встановити та підтвердити наявність біохімічних змін з боку ліпідного обміну та вмісту ЦІК у пацієнтів iз запальними захворюваннями кишечника.
Цель: определить уровень циркулирующих иммунных комплексов (ЦИК) и состояние липидного обмена у пациентов с возрастными и гендерными особенностями протекания воспалительных заболеваний кишечника (ВЗК). Материалы и методы. Проведено обследование 80 пациентов с ВЗК: 53 с неспецифическим язвенным колитом (НЯК) и 27 с болезнью Крона (БК). Они были разделены на две группы в зависимости от пола: 40 мужчин и 40 женщин. Кроме того, все больные были разделены на группы в зависимости от возраста: молодые (45 человек — 28 с НЯК и 17 с БК); среднего возраста (15 пациентов — 10 с НЯК и 5 с БК); пожилые (20 человек — 15 с НЯК и 5 с БК). Контрольную группу составили 20 практически здоровых людей. В сыворотке крови определяли уровень ЦИК, общего холестерина, триглицеридов, холестерина липопротеинов высокой, низкой и очень низкой плотности (ЛПОНП), коэффициент атерогенности. Результаты. Уровень ЦИК в сыворотке крови достоверно превышал норму у женщин с ВЗК — в 1,57 раза (р < 0,05), что можно рассматривать как показатель интенсивности воспаления, вовлечения иммунной системы в патологический процесс. У женщин с НЯК уровень ЦИК достоверно повышен — в 1,62 раза (р < 0,05) по сравнению с контрольной группой. При ВЗК содержание ЦИК зависело от возраста больных, оно было достоверно повышено — в 1,5 раза (р < 0,05) и 1,4 раза (р < 0,05) у пациентов среднего и пожилого возраста соответственно в сравнении с молодыми больными. Установлена корреляция между уровнем ЦИК и возрастом (r = +0,552; р = 0,025). Выявлено нарушение липидного обмена у женщин с НЯК, что выражалось в снижении уровня триглицеридов в сыворотке крови в 1,7 раза (р < 0,001), а у мужчин с БК происходило уменьшение данного показателя в 1,5 раза (р < 0,05) по сравнению с контрольной группой. У женщин с НЯК достоверно снижался уровень ЛПОНП в сыворотке крови — в 2 раза (р < 0,05), а у мужчин с БК — в 1,8 раза (р < 0,05) по сравнению с контрольной группой. Установлено достоверное уменьшение уровня триглицеридов — в 1,5 раза (р < 0,05) и в 1,6 раза (р < 0,05) у молодых пациентов с НЯК и БК соответственно и в 1,6 раза (р < 0,05) у пациентов среднего возраста с БК. Параллельно наблюдалась выраженная тенденция к снижению уровня холестерина у всех молодых пациентов с ВЗК. Установлено достоверное уменьшение коэффициента атерогенности у молодых больных. Выводы. Проведенные исследования позволили установить и подтвердить наличие биохимических изменений со стороны липидного обмена и уровня ЦИК у пациентов с воспалительными заболеваниями кишечника.
Background. The purpose of the present work was to assess the level of circulating immune complexes (CIC) and lipid metabolism state in patients with inflammatory bowel disease (IBD). Materials and methods. We examined 80 patients with IBD: 53 with ulcerative colitis (UC) and 27 with Crohn’s disease (CD). Depending on the gender, they were divided into two groups: 40 womеn and 40 men. Also, depending on the age, all patients were divided into three groups: young (45 individuals — 28 with UC and 17 with CD); middle-aged (15 persons — 10 with UC and 5 with CD); elderly (20 patients — 15 with UC and 5 with CD). The control group included 20 apparently healthy individuals. In patients’ blood serum, the levels of CIC, total cholesterol, triglycerides, phospholipids, high-density, low-density and very low-density lipoprotein cholesterol were determined, as well as atherogenic index. Results. Serum level of CIC significantly exceeded the normal values in women with IBD — by 1.57 times (p < 0.05), which can be considered as an indicator of inflammation intensity, involvement of the immune system in the pathological process. In women with UC, the content of CIC was significantly increased — by 1.62 times (p < 0.05) compared to the control group. In IBD, the level of CIC depended on the age of patients; it was significantly increased — by 1.5 times (p < 0.05) and 1.4 times (p < 0.05) — in middle-aged patients and in the elderly, respectively, compared to a group of young patients. The correlation between the level of CIC and the age (r = +0.552; p = 0.025) was established. The violation of lipid metabolism was observed in women with UC, which manifested in 1.7-time reduction of serum triglycerides (p < 0.001); in men with CD, a decrease in this indicator by 1.5 times (p < 0.05) occurred compared to the control group. In women with UC, the serum level of very low-density lipoproteins was 2 times lower (p < 0.05), and in men with CD — 1.8 times (p < 0.05) as compared to controls. A probable reduction in the content of triglycerides was detected: by 1.5 times (p < 0.05) and 1.6 times (p < 0.05) in young patients with UC and CD, respectively, and by 1.6 times (p < 0.05) in middle-aged patients with CD. In parallel, there was a pronounced tendency to cholesterol lowering in all young patients with IBD. A probable decrease in the atherogenic index was detected in young patients. Conclusions. The completed studies allowed establishing and confirming the presence of biochemical changes in patients with IBD (lipid metabolism and the content of CIC), which play the main role in the pathogenetic mechanisms of these diseases.
запальні захворювання кишечника; неспецифічний виразковий коліт; хвороба Крона; циркулюючі імунні комплекси; ліпідний обмін
воспалительные заболевания кишечника; неспецифический язвенный колит; болезнь Крона; циркулирующие иммунные комплексы; липидный обмен
inflammatory bowel diseases; ulcerative colitis; Crohn’s disease; circulating immune complexes; lipid metabolism
Introduction
Inflammatory bowel diseases (IBD), which include ulcerative colitis (UC) and Crohn’s disease (CD), remain one of the most complex problems of gastroenterology. Constant recurrent course with a progressive violation of the structure and functions of the intestinal mucosa is accompanied by a significant decrease in the patient’s quality of life that makes IBD one of important medical and social problems and involves search for new directions in studying the etiology and pathogenesis in order to improve methods for the prevention and treatment of this pathology [1, 2]. The continued interest of scientists in this pathology is associated with an increase in IBD morbidity all over the world. According to some scientists, this situation is due to anthropogenic pollution of the biosphere and environment, urbanization, growing influence of adverse external factors, number of allergens in food, high degree of sensitization of the population, dietary habits, widespread use of alcohol and other factors, and it leads to an increase not only in the frequency of IBD, but also in the number of severe cases, common forms of the disease, extraintestinal lesions and complications of IBD [3].
In the last decade, the extension of methodological possibilities, the introduction of functional and morphological methods of research have greatly deepened the understanding of the etiology and pathogenesis of chronic intestinal diseases and made it possible to develop recommendations for their diagnosis and treatment. However, many issues of clinical and pathogenetic features of the course of this nosology are not fully resolved, the effectiveness of treatment is insufficient that contributes to the formation of resistant forms of diseases, decrease in the quality of life and loss of efficiency. This encourages the search for the mechanisms of intestinal pathology, which can be associated with extraorganic causes [4, 5].
It is known that the basis of IBD pathogenesis is a violation of the immune response, which leads to the development of nonspecific inflammation in the intestinal walls and mucosa. The effect of circulating immune complexes (CIC) and inflammatory mediators (cytokines, histamine, reactive oxygen species, nitric oxide) on the cells of the intestinal wall lead to its damage and tissue degradation [6, 7].
Violation of the intestinal mucosal barrier, increased antigen loading, damage to the cytokine link of homeostasis, activation of immune cells, excess synthesis of CIC can cause the formation of extraintestinal lesions in IBD [8].
CIC is the physiological product of the antigen-antibody reaction, which is a part of the protective immune mechanisms of the body. The formation of immune complexes is an integral indicator of the development of humoral immune response. Some content of immune complexes should be constantly present in the blood for the implementation of physiological processes of homeostasis. Moreover, this indicates an adequate body response to external influences. But it should be noted that with excessive accumulation of CIC due to increased production or lack of their removal from the body, a transition to the pathology is possible that is caused by an increase in the biological activity of immune complexes, and, under special conditions, they can play an important role in the pathogenesis of autoimmune processes [5].
The role of lipids in the physiological processes and in the development of pathological conditions, together with many other factors, depends on their qualitative composition. These characteristics are determined by many processes: synthesis, catabolism, plasma elimination, qualitative features of protein and lipid components. The state of these processes, in turn, is due to the condition of the digestive tract, especially the liver as one of the main organs that regulates the substrate-enzymatic relationship in lipid metabolism [6, 9]. Previously, we have shown that in patients with IBD, the total content of free fatty acids in the blood serum was significantly increased as compared to controls, precisely at the expense of polyunsaturated fatty acids, especially in middle-aged patients, which may be due to the activation of inflammatory processes, immune responses, and also to the enhanced lipid peroxidation [9].
The purpose of the work was to assess the level of circulating immune complexes and lipid metabolism state in patients with inflammatory bowel diseases.
Materials and methods
Eighty patients with IBD (53 with UC and 27 with CD) were examined at the department of bowel diseases of the Institute of Gastroenterology of the National Academy of Medical Sciences of Ukraine in 2017–2018.
Depending on the gender, patients were divided into two groups: 40 womеn and 40 men. Also, depending on the age, all patients were divided into three groups: young (45 individuals — 28 with UC and 17 with CD); middle-aged (15 persons — 10 with UC and 5 with CD); elderly (20 patients — 15 with UC and 5 with CD). The control group included 20 apparently healthy individuals.
The level of CIC in patients’ blood serum was determined according to V. Haskova technique.
Such biochemical parameters as total cholesterol (TC), triglycerides (TG), phospholipids, high-density (HDL), low-density (LDL) and very low-density lipoprotein (VLDL) cholesterol, atherogenic index (AI) were analysed with Cormay test-kits (Poland) and biochemical analyzer Stat Fax 1904 Plus (Awareness Technology, USA) and calculated according to Friedewald formula. The normal TC levels were 2.96–4.4 mmol/l, TG — 0.40–0.9 mmol/l, HDL — 0.99–1.59 mmol/l, LDL — 1.63–2.59 mmol/l and VLDL — 0.22–0.40 mmol/l.
Descriptive statistics was used for statistical analysis of the data; the comparison of the mean values of variables was carried out using parametric methods (Student’s t-test) for the normal distribution of the data measured on the interval scale. The correspondence of the characteristics of distribution to the normal distribution law was verified using the Shapiro-Wilk test. In other cases, a non-parametric method was used (Mann-Whitney U-test). To compare the particle distribution of two or more variables, the χ2 test was used. Correlation analysis was performed by Pearson (for data measured on the interval scale) and Spearman coefficients (for data not measured on the interval scales). All calculations were performed in SPSS 9.0 for Windows.
Results and discussion
The content of the CIC in patients with IBD was 0.8–14.5 optical density units. The average levels were (4.82 ± 0.42) optical density units in men and (5.37 ± 0.49) optical density units in women. The CIC level in 65.0 % of women and in 57.5 % of men with IBD exceeded that of control group. There is no statistically significant difference between the level of CIC in men and women.
When analysing the indicator depending on the nosology, it was found that in women with IBD, the level of CIC was significantly increased compared to the control group — by 1.57 times (p < 0.05). In women with UC, the level of CIC was significantly increased — by 1.62 times (p < 0.05) compared to the control group.
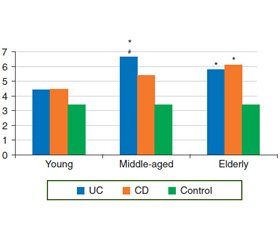
The analysis of indicators was performed depending on the age of patients (Fig. 1). A possible increase in the serum level of CIC was observed in 80.0 % of middle-aged and in 70.0 % of elderly patients, indicating active inflammatory process. The highest level of CIC was found in the group of middle-aged patients with UC (a 1.9-time increase compared to controls, p < 0.05).
It was found that the level of CIC increased with increasing age of patient, which was confirmed by the established correlation between the level of CIC and age (r = +0.552; p = 0.025). So, their level is probably increased by 1.5 times (p < 0.05) and 1.4 times (p < 0.05) in middle-aged patients and in the elderly with IBD, respectively, in comparison with the group of young patients.
In the general group of patients with IBD (men and women, young and middle-aged patients), the following changes in serum lipid metabolism were observed: a probable decrease in TG content by 1.5 times ((0.76 ± 0.06) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.05), LDL — by 1.8 times ((0.36 ± 0.05) mmol/l vs. (0.65 ± 0.14) mmol/l, p < 0.05) and a tendency to decrease in the content of TC, HDL, LDL compared with controls.
The results of biochemical studies of lipid metabolism indicators in the blood serum of patients with IBD depending on gender are presented in Table 1. As you can see, there was a probable decrease in serum TG level of women in the general group of IBD — by 1.6 times ((0.71 ± 0.07) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.01), and in UC — by 1.7 times ((0.66 ± 0.07) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.001). In men with IBD, especially with CD, there was also a probable decrease in the TG content — by 1.4 times ((0.84 ± 0.09) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.05) and by 1.5 times, respectively ((0.78 ± 0.11) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.05). Probably, a decrease in TG level may indirectly indicate a violation of the cell membrane structure and malabsorption of these fats in the small intestine.
A clear downward trend in HDL serum levels was determined in men with IBD, unlike women, whose indicator was slightly different from the control group (Table 1). Decreased HDL levels indicate a violation of the transport of excess lipids from the blood to the liver.
A probable difference in the content of LDL that play a major role in the formation of atherosclerotic plaques was not observed in patients with IBD compared to the control group. Analysis of nosologies showed similar changes in both UC and CD (Table 1).
A probable 2-fold decrease in the serum content of VLDL ((0.32 ± 0.03) mmol/l vs. (0.65 ± 0.14) mmol/l, p < 0.05) was determined in women with IBD and 2.2-fold — in women with UC ((0.30 ± 0.03) mmol/l vs. (0.65 ± 0.14) mmol/l, p < 0.05). In men with CD, there was a probable 1.8-time decrease in VLDL content ((0.36 ± 0.05) mmol/l vs. (0.65 ± 0.14) mmol/l, p < 0.05). They transport 5–10 times more TG than cholesterol esters. The risk of atherosclerosis developing increases with increased levels of VLDL and LDL in the blood, as well as with low HDL contents.
AI was significantly lower in women with IBD — by 1.2 times ((2.13 ± 0.15) mmol/l vs. (2.55 ± 0.09) mmol/l, p < 0.05), with UC — by 1.3 times ((1.99 ± 0.16) mmol/l vs. (2.55 ± 0.09) mmol/l, p < 0.01) compared to controls. In men, AI changes were non-significant. AI is an integral indicator that allows you to accurately predict the risk of atherosclerosis developing. High atherogenicity is determined by the presence of LDL fraction. HDL fraction is antiatherogenic.
There was a probable decrease in the serum TG levels in young patients with IBD — by 1.5 times ((0.75 ± 0.07) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.05) and in middle-aged patients with CD — by 1.6 times ((0.73 ± 0.12) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.05) against the general downward trend in TG content in these age groups compared to controls.
It is important to note a probable TG decrease in middle-aged patients with CD by 1.6 times ((0.70 ± 0.12) mmol/l vs. (1.15 ± 0.12) mmol/l, p < 0.05). In the blood of elderly patients, there were no significant changes in TG content in contrast to controls, but it tended to increase compared to young and middle-aged.
There were no significant changes in the content of TC, HDL, LDL in patients of all age groups. A probable 1.9-time decrease was noted in VLDL of young patients with IBD, UC and CD, and 2-fold — in the middle-aged patients with IBD and CD compared to the control group.
AI was significantly lower in young patients (2.04 ± 0.10; 1.96 ± 0.12 vs. 2.55 ± 0.09, p < 0.001, respectively, for IBD and UC) as compared to controls. In middle-aged patients, there was a tendency to AI increase, especially in persons with UC. In middle-aged patients and in the elderly, AI was within the normal range.
The results show that in patients with IBD, the level of CIC depended on age, so in patients of middle and advanced age, it was probably higher than in young ones, and a high level of CIC indicated that the macrophage system does not eliminate the antigen-antibody complex.
Thus, the detected changes of total serum lipids indicate metabolic disorders and the presence of energy insufficiency regardless of gender or age characteristics, which may be due to disorders of neutral fats digestion and malabsorption of food products in the small intestine. A 1.2-time decrease in the total serum cholesterol in the general group of patients with IBD allowed assuming that there are violations in the structure of cell membranes.
The completed studies allowed establishing and confirming the presence of biochemical changes (lipid metabolism and the content of CIC) in patients with inflammatory bowel diseases that play the main role in the pathogenetic mechanisms of these diseases, have their clinical manifestations and need therapeutic correction.
Conclusions
1. Serum level of CIC significantly exceeded the normal values in women with IBD — by 1.57 times (p < 0.05), which can be considered as an indicator of inflammation intensity, involvement of the immune system in the pathological process. In women with UC, the level of CIC was significantly increased — by 1.62 times (p < 0.05) compared to the control group. In IBD, the level of CIC depended on the age of these patients. Its level is significantly increased — by 1.5 times (p < 0.05) and 1.4 times (p < 0.05) in middle-aged patients and in the elderly, respectively, compared to a group of young patients. The correlation between the level of the CIC and the age (r = +0.552; p = 0.025) was established.
2. The violation of lipid metabolism was observed in women with ulcerative colitis, which manifested in 1.7-time reduction in the serum triglycerides (p < 0.001), and in men with Crohn’s disease, there was a 1.5-time decrease in this indicator (p < 0.05) compared to the control group. In women with ulcerative colitis, the level of very low-density lipoproteins was 2 times lower (p < 0.05), and in men with Crohn’s disease — 1.8 times (p < 0.05) lower compared to controls.
3. There was a probable reduction in triglyceride content — by 1.5 times (p < 0.05) and 1.6 times (p < 0.05) in young patients with ulcerative colitis and Crohn’s disease, respectively, and by 1.6 times (p < 0.05) in middle-aged patients with Crohn’s disease. In parallel, there was a clear downward trend to cholesterol lowering in all young patients with inflammatory bowel diseases. A probable decrease in the atherogenic index is determined in young patients.
Conflicts of interest. Authors declare no conflicts of interests that might be construed to influence the results or their manuscript.
1. Бойко Т.И. Состояние функции сосудистого эндотелия у больных с хроническими воспалительными заболеваниями / Т.И. Бойко, М.В. Стойкевич, Е.В. Колбасина, Е.В. Сорочан // Сучасна гастроентерологія. — 2010. — № 1(51). — С. 5-10.
2. Степанов Ю.М. Хронічні запальні захворювання кишечника: особливості епідеміології в Україні / Ю.М. Степанов, І.Ю. Скирда, О.П. Петішко // Гастроентерологія. — 2017. — Т. 51, № 2. — С. 11-19. http://dx.doi.org/10.22141/2308-2097.51.2.2017.101703.
3. Носова І.А. Труднощі діагностики та обґрунтування принципів базисного лікування хворих на неспецифічні запальні хвороби кишечнику // Сучасна гастроентерологія. — 2007. — № 4(36). — С. 51-55.
4. Пасієшвілі Л.М. Хронічний коліт як чинник розвитку та прогресування вторинного остеопорозу у хворих з остеохондрозом хребта / Л.М. Пасієшвілі, А.Б. Андруша // Сучасна гастроентерологія. — 2008. — № 2. — C. 30-33.
5. Вдовиченко В.І. Порівняльна характеристика мікробіоценозу кишечнику у хворих на синдром подразненого кишечнику та неспецифічний виразковий коліт / В.І. Вдовиченко, О.П. Корнійчук, О.О. Меренцова, Ю.С. Лозинський // Сучасна гастроентерологія. — 2010. — № 4(54). — С. 67-70.
6. Татьянина O.Ф. Маркеры кишечного воспаления при заболеваниях кишечника: обзор литературы / О.Ф. Татьянина, А.С. Потапов, Л.С. Намазова, Е.Г. Цимбалова, А.Г. Кучеренко, А.Н. Сурков // Педиатрическая фармакология. — 2008. — Т. 5, № 3. — С. 39-45.
7. Стeпанов Ю.М. Содержание фекального кальпротектина у больных хроническими воспалительными заболеваниями кишечника / Ю.М. Степанов, Н.С. Федорова // Сучасна гастроентерологія. — 2010. — № 2. — С. 44-48.
8. Дорофєєв А.Е. Ураження гепатобіліарної системи при неспецифічному виразковому коліті та хворобі Крона / А.Е. Дорофєєв, Н.В. Драгомирицька, Г.М. Іжа, О.О. Россохіна // Університетська клініка. — 2013. — Т. 9, № 2. — С. 228-230.
9. Калинкина Н.В. Особенности метаболизма оксида азота под влиянием различных кумулятивных доз антрациклиновых препаратов: Автореф. дис… канд. мед. наук: 14.01.11. — Донецк, 2010. — 6 с.

/52-2.jpg)
/52-1.jpg)