Журнал "Гастроэнтерология" Том 53, №2, 2019
Вернуться к номеру
Стан ендогенної інтоксикації та імунозапальної реакції у хворих на алкогольний цироз печінки в поєднанні з неалкогольною жировою хворобою печінки
Авторы: N.R. Matkovska(1), N.H. Virstiuk(1), U.V. Balan(1, 2)
(1) — Ivano-Frankivsk National Medical University, Ivano-Frankivsk, Ukraine
(2) — Ivano-Frankivsk Regional Clinical Hospital, Ivano-Frankivsk, Ukraine
Рубрики: Гастроэнтерология
Разделы: Клинические исследования
Версия для печати
Мета: оцінити стан ендогенної інтоксикації у хворих на алкогольний цироз печінки (АЦП) при поєднанні з неалкогольною жировою хворобою печінки (НАЖХП) залежно від стадії декомпенсації. Матеріали та методи. Обстежено 204 пацієнти. Серед них у 78 осіб (І група) діагностовано АЦП та в 126 осіб (ІІ група) було поєднання АЦП з НАЖХП. Пацієнтів було поділено на підгрупи залежно від класів компенсації за критеріями Чайлда — П’ю (А, В, С). Проведено загальноклінічні та інструментальні обстеження. Визначали лейкоцитарний індекс інтоксикації (ЛІІ), сорбційну здатність еритроцитів (СЗЕ), рівень резистину, високочутливого С-реактивного білка (вч-СРБ) і фактора некрозу пухлини α (ФНП-α) у крові. Результати. У пацієнтів із поєднанням АЦП та НАЖХП спостерігалася більш тяжка клінічна картина з розвитком астеновегетативного, больового, диспептичного, гепаторенального, гепатопульмонального синдромів, жовтяниці, портальної гіпертензії, печінкової енцефалопатії. Відмiчалися такі тяжкі інфекційні ускладнення, як пневмонія і спонтанний бактеріальний перитоніт, частіше в пацієнтів із субкомпенсацією та декомпенсацією. В усіх хворих СЗЕ, ЛІІ i показники ФНП-α, вч-СРБ та резистину збільшувалися з наростанням декомпенсації захворювання. Підвищені СЗЕ, ЛІІ й вищі рівні ФНП-α, вч-СРБ та резистину в сироватці крові спостерігалися при поєднанні АЦП та НАЖХП, що пов’язане з більш тяжким перебігом патологічного стану в таких хворих. Ми виявили позитивні зв’язки між рівнем резистину та ФНП-α, вч-СРБ, СЗЕ, ЛІІ. Такі результати свідчать про участь резистину в імунозапальних процесах та розвитку ендогенної інтоксикації при АЦП. Висновки. З наростанням декомпенсації АЦП при поєднанні з НАЖХП збільшується ступінь ендогенної інтоксикації, яка супроводжується розвитком імунозапальної реакції, про що свідчать підвищені СЗЕ, ЛІІ, а також вищі рівні ФНП-α, вч-СРБ та резистину. Вірогідно вищі СЗЕ, ЛІІ i рівні ФНП-α, вч-СРБ та резистину виявлено у хворих при поєднанні АЦП з НАЖХП, що супроводжується більш тяжким перебігом захворювання. У пацієнтів iз АЦП та НАЖХП виявлено кореляції між рівнем резистину та ФНП-α, вч-СРБ, СЗЕ, ЛІІ.
Цель: оценить состояние эндогенной интоксикации у пациентов с алкогольным циррозом печени (АЦП) при сочетании с неалкогольной жировой болезнью печени (НАЖБП) в зависимости от стадии декомпенсации. Материалы и методы. Обследовано 204 пациента. Среди них у 78 человек (I группа) диагностирован АЦП и у 126 лиц (II группа) было сочетание АЦП с НАЖБП. Пациентов разделили на подгруппы в зависимости от классов компенсации по критериям Чайлда — Пью (А, В, С). Проведены общеклинические и инструментальные обследования. Определяли лейкоцитарный индекс интоксикации (ЛИИ), сорбционную способность эритроцитов (ССЭ), уровень резистина, высокочувствительного С-реактивного белка (вч-СРБ) и фактора некроза опухоли α (ФНО-α) в крови. Результаты. У пациентов с сочетанием АЦП и НАЖБП наблюдалась более тяжелая клиническая картина с развитием астеновегетативного, болевого, диспептического, гепаторенального, гепатопульмонального синдромов, желтухи, портальной гипертензии, печеночной энцефалопатии. Отмечались такие тяжелые инфекционные осложнения, как пневмония и спонтанный бактериальный перитонит, чаще у пациентов с субкомпенсацией и декомпенсацией. У всех больных ССЭ, ЛИИ и показатели ФНО-α, вч-СРБ, резистина увеличивались с нарастанием декомпенсации заболевания. Повышенные ССЭ, ЛИИ и более высокие уровни ФНО-α, вч-СРБ и резистина в сыворотке крови наблюдались при сочетании АЦП и НАЖБП, что связано с более тяжелым течением патологического состояния у таких больных. Мы обнаружили положительные связи между уровнем резистина и ФНО-α, вч-СРБ, ССЭ, ЛИИ. Такие результаты свидетельствуют об участии резистина в иммуновоспалительных процессах и развитии эндогенной интоксикации при АЦП. Выводы. С нарастанием декомпенсации АЦП при сочетании с НАЖБП увеличивается степень эндогенной интоксикации, которая сопровождается развитием иммуновоспалительной реакции, о чем свидетельствуют повышенные ССЭ, ЛИИ, а также более высокие уровни ФНО-α, вч-СРБ и резистина. Достоверно более высокие ССЭ, ЛИИ и уровни ФНО-α, вч-СРБ и резистина выявлены у больных при сочетании АЦП с НАЖБП, что сопровождается более тяжелым течением заболевания. У пациентов с АЦП и НАЖХП обнаружены корреляции между уровнем резистина и ФНО-α, вч-СРБ, ССЭ, ЛИИ.
Background. The purpose was to evaluate the state of endogenous intoxication and immune-inflammatory response in patients with alcoholic liver cirrhosis (ALC) associated with non-alcoholic fatty liver disease (NAFLD), depending on the stage of decompensation. Materials and methods. The study included 204 patients. Among them, 78 patients were diagnosed with alcoholic liver disease at the stage of liver cirrhosis (group I) and 126 patients had a combination of ALC and NAFLD (group II). General-clinical and instrumental examinations were performed. The leukocyte index of intoxication (LII), sorption capacity of erythrocytes (SCE), levels of resistin, highly sensitive C-reactive protein (hs-CRP) and tumor necrosis factor α (TNFα) in the blood were determined. Results. Patients with a combination of ALC and NAFLD had a more severe clinical picture with the development of astheno-vegetative, pain, dyspeptic, hepatorenal, hepatopulmonary syndromes, jaundice, portal hypertension, liver encephalopathy. Among severe infectious complications, pneumonia and spontaneous bacterial peritonitis were more common in persons with subcompensation and decompensation. In all patients, SCE, LII, TNFα, hs-CRP and resistin levels increased with increasing decompensation of the disease. Higher SCE, LII, TNFα, hs-CRP and resistin levels were observed in patients with ALC associated with NAFLD due to a more severe course of the pathological condition. Positive correlations were found between resistin level and TNFα, hs-CRP, SCE, and LII. Conclusions. Analyzing the results of the study, it was found that with an increase in ALC decompensation, the degree of endogenous intoxication, which is accompanied by the development of immune-inflammatory response, is increasing, as evidenced by elevated SCE, LII, TNFα, hs-CRP, and resistin levels. Significantly higher SCE, LII, TNFα, hs-CRP, and resistin levels were detected in patients with a combination of ALCs and NAFLD accompanied by a more severe course of the disease. In patients with ALC associated with NAFLD, correlation between the resistin level and SCE, LII, TNFα, hs-CRP was found.
алкогольна хвороба печінки; неалкогольна жирова хвороба печінки; цироз печінки; ендогенна інтоксикація; імунозапальна реакція
алкогольная болезнь печени; неалкогольная жировая болезнь печени; цирроз печени; эндогенная интоксикация; иммуновоспалительная реакция
alcoholic liver disease; non-alcoholic fatty liver disease; liver cirrhosis; endogenous intoxication; immune-inflammatory response
Introduction
Non-alcoholic fatty liver disease (NAFLD) is one of the most common liver diseases characterized by the progression of the course and the development of severe complications. It is detected in 20–35 % of the adult population, both in industrialized and developing countries, as well as in 40–70 % of obese patients [1]. Today, it is believed that NAFLD is a hepatic manifestation of metabolic syndrome, since its prevalence is associated with an increase in obesity and type 2 diabetes at the general population level [2, 3]. Visceral obesity, which is typical for metabolic syndrome, is associated with a decrease in insulin sensitivity, hyperglycemia, dyslipidemia, hypertension, prothrombotic and proinflammatory conditions [4, 5]. NAFLD is more often described as a component of combined pathology. It is detected mostly in cardiovascular and endocrine pathologies. NAFLD is considered a risk factor for cardiovascular diseases and a predictor of cardiovascular complications [6, 7].
NAFLD is characterized by excessive accumulation of hepatic fat and is determined by the steatosis in more than 5 % of hepatocytes, has a long asymptomatic course [8]. The pathogenesis of NAFLD is multifactorial. High consumption of fructose and fat, insulin resistance, immune-inflammatory processes, lipotoxicity, genetic predisposition and imbalance of intestinal microbiota are the factors for the development and progression of the disease [9]. The liver interacts closely with fatty tissue, which is not only an energetic but also a powerful endocrine organ that expresses and produces a large number of biologically active polypeptides — adipokines. They act both on the local (autocrine and paracrine) and on the systemic (endocrine) level. Among the cytokines and related proteins with endocrine function, the most well-known are leptin, tumor necrosis factor α (TNFα), interleukin-6 (IL-6), monocyte chemoattractant protein-1 (MCP-1), visfatin, chemerin; among fibrinolytic proteins — plasminogen activator inhibitor-1 (PAI-1), tissue factors; among complement components and associated proteins — adipsin (or complement D factor), adiponectin, acylation-stimulating protein (ASP); among the lipids and proteins that influence lipid metabolism or transport — lipoprotein lipase, cholesteryl ester transfer protein, apolipoprotein E, non-esterified serum fatty acids; cytochrome P450-dependent aromatase and 17-β-hydroxysteroid dehydrogenase are the enzymes involved in steroid metabolism; among proteins of renin-angiotensin system, the most well-known is angiotensinogen; among other proteins — resistin, apelin, retinol-binding protein, obestatin, omentin, vaspin and others. In adipose tissue, a large number of receptors is expressed, including insulin, glucagon, thyroid-stimulating hormone, glucocorticoid, androgenic, estrogenic, progesterone, leptin, apelin, IL-6 receptors, TNFα, gastrin/cholecystokinin-B, glucagon-like peptide-1, growth hormone, vitamin D, thyroid hormone, catecholamines and angiotensin II (type 1 and type 2). They are involved in various processes, including inflammation, immunological reactions, insulin sensitivity, liver steatosis and steatohepatitis [10–12].
The publications of recent years show an ambiguous role of resistin in the pathogenesis of NAFLD. Adipokine was discovered in 2001 and was called the insulin resistance hormone. However, it is secreted mainly by macrophages and, to a lesser extent, by fatty tissue. In addition to the differentiation of adipocytes, inhibition of adipogenesis and glucose uptake by cells, adipokine affects the stimulation of inflammatory mechanisms, activation of the endothelium, and proliferation of smooth muscle cells in the blood vessels [6, 12].
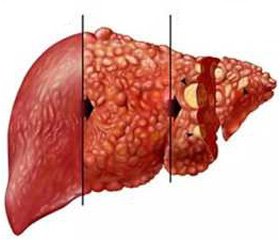
The initial manifestations of NAFLD are fatty hepatoses with a predominance of fatty liver dystrophy, steatohepatitis with severe inflammatory infiltrates both in the stroma and in the parenchyma, focal necrosis, steatofibrosis with predominant localization in the portal stroma. However, under adverse conditions, the pathological process is transformed into the liver cirrhosis (LC) and may lead to hepatocellular carcinoma. The basis for the development of LC are the processes of fibrosis, necrosis, angiogenesis, which through the cascade of systemic metabolic and immune-inflammatory responses lead to endotoxemia, restructuring of the normal structure of the parenchyma and the vascular system of the liver with the formation of pseudolobules, regenerative nodules and the development of multiple organ failure [13, 14].
It is believed that pathogenetic links in the development of NAFLD and alcoholic liver disease (ALD) are similar, although they have different etiologic factors. Often, NAFLD develops along with ALD, causing systemic lipid, carbohydrate and protein metabolism disorders. This combination, especially at the stage of LC, becomes prognostically unfavourable for patients and leads to systemic complications, irritability and progression.
The purpose was to evaluate the state of endogenous intoxication and immune-inflammatory response in patients with alcoholic liver cirrhosis associated with NAFLD, depending on the stage of decompensation.
Materials and methods
The study included 204 patients with diagnosed liver cirrhosis who underwent inpatient treatment at the gastroenterology department of the Ivano-Frankivsk Regional Clinical Hospital. Among them, 78 patients were diagnosed with ALD at the stage of LC (group I) and 126 patients had a combination of alcoholic liver cirrhosis (ALC) and NAFLD (group II). Group I included 24 women and 54 men aged (53.2 ± 11.4) years with average duration of the disease (5.9 ± 2.1) years; group II — 22 women and 104 men aged (47.8 ± 9.4) years, average duration of the disease was (4.2 ± 2.7) years. All patients were divided in subgroups depending on LC compensation by the Child-Pugh score: IA (n = 17), ІВ (n = 38), IC (n = 23); IIA (n = 44), ІІВ (n = 48), ІІС (n = 34). The diagnosis was verified using clinical and laboratory-instrumental methods in accordance with the Order of the Ministry of Health of Ukraine No. 826 dated November 06, 2014, adapted clinical guidelines “Non-Alcoholic Fatty Liver Disease”, adapted clinical guidelines “Alcoholic Liver Disease” (2014), adapted clinical guidelines “Cirrhosis of the Liver” (2017) (State Expert Centre of the Ministry of Health of Ukraine, Ukrainian Gastroenterology Association, Kyiv), recommendations of the European Association for the Study of Liver, Diabetes and Obesity (2016) [15].
General clinical examinations, ultrasound examination of the abdominal cavity, esophagogastroduodenoscopy were performed. To detect the alcoholic etiology of the disease, according to the recommendations of the World Health Organization, more than 2 doses of alcohol (1 standard dose = 10 g of pure alcohol) per day for women and more than 4 doses for men were taken into account. CAGE (Cut, Annoyed, Guilty, Eye-opener) questionnaire, AUDIT (Alcohol Use Disorders Identification Test, 1989), PAS (post-alcohol syndrome) questionnaire developed by P.P. Ogurtsov, A.B. Pokrovsky, A.E. Uspensky, LeGo (P.M. LeGo, 1976) in the modification of O.B. Zharkov, 2000, ANI (Alcoholic liver disease/nonalcoholic fatty liver disease index, 2006) were used. The control group included 20 age- and sex-matched apparently healthy persons.
Exclusion criteria were liver cirrhosis of the viral, toxic, autoimmune origin, metabolic diseases of the liver, cancer, and no individual consent of the patient to conduct the study. All patients were matched for age and sex. The research was carried out in accordance with the ethical principles of conducting scientific research, principles of the Declaration of Helsinki.
The degree of endogenous intoxication was determined by the leukocyte index of intoxication (LII) calculated according to the Kal-Kalif formula: LII = [(4Mc + 3Yu + + 2S + M) × (Pl + 1)] / [(Lymph + Mon) × (E + 1)], where Mc — myelocytes, Yu — young, S — stab, M — microxyphil, Pl — plasma cells, Lymph — lymphocytes, Mon — monocytes, E — eosinophils, and by the test of sorption capacity of erythrocytes (SCE). The basis of the SCE test is the ability of the red blood cells (as a universal absorbent) to absorb the vital stain (0.025% solution of methylene blue), which is determined by the photocolorimeter, and corresponds to the degree of endogenous intoxication. In the control group, SCE was (27.30 ± 1.56) %. The activity of the inflammatory process was evaluated by the content of high-sensitivity C-reactive protein (hs-CRP) and TNFα in the blood, which was determined using ELISA kit (Elabscience, USA), Human hs-CRP, Human TNF-alpha High Sensitivity ELISA (Biovendor, Czech Republic) according to manufacturer’s techniques. Resistin level was determined by immunoassay using the Resistin Human ELISA kit (Biovendor, Czech Republic). In the control group, the levels of hs-CRP, TNFα and resistin were (0.65 ± 0.02) mg/l, (17.38 ± 1.15) pg/ml and (3.72 ± 0.26) ng/ml, respectively.
Statistical analysis. Statistical processing of the obtained results was carried out using the software package Statistica v. 12.0 (StatSoft, USA) and Microsoft Excel. The arithmetic average (M) and the standard deviation (SD) were used as the rates of parametric statistics. To determine the significance of the differences between the groups in the distribution close to normal, Student’s t-test was used. For the analysis of dependencies, a method of correlation analysis with the Spearman’s rank correlation coefficient was used. Differences were considered statistically significant at p < 0.05.
Results
Clinically, the signs of astheno-vegetative syndrome were detected in 29.4 (5 of 17), 45.4 % (20 of 44), 57.9 % (22 of 38), 79.2 % (38 of 48), 100 % (23) and 100 % (34) of persons of IA, ІІА, ІB, ІІB, ІС and ІІС groups, respectively; pain syndrome — in 11.8 % (2 of 17), 27.3 % (12 of 44), 34.2 % (13 of 38), 43.6 % (21 of 48), 100 % (23) and 100 % (34) of patients of the above-mentioned groups, respectively; dyspeptic syndrome — in 23.5 % (4 of 17), 75 % (33 of 44), 68.4 % (26 of 38), 91.7 % (44 of 48), 100 % (23) and 100 % (34) of individuals, respectively; hepatorenal syndrome — in 31.8 % (14 of 44), 10.5 % (4 of 38), 60.4 % (29 of 38), 78.3 % (18 of 48), 100 % (34) of persons in ІІА, ІВ, ІІВ, ІС and ІІС groups, respectively; hepatopulmonary syndrome — in 17.6 % (3 of 17), 40.9 % (18 of 44), 21.1 % (8 of 38), 52.1 % (25 of 48), 82.6 % (19 of 23) and 100 % (34) of patients of ІА, ІІА, ІВ, ІІВ, ІС and ІІС groups, respectively; jaundice — in 17.6 % (3 of 17), 45.4 % (20 of 44), 73.7 % (28 of 38), 95.8 % (46 of 48) and 100 % (23) of individuals of ІА, ІІА, ІВ, ІІВ, ІС and ІІС groups, respectively; medically uncontrolled ascites — in 47.8 % (11 of 23) and 67.6 % (23 of 34) in IC and ІІС groups; clinical signs of hepatic encephalopathy — in 52.9 % (9 of 17), 86.4 % (38 of 44) of persons of IA, ІІА groups and in all patients of ІВ, ІІВ, ІС and ІІС groups, respectively (Table 1). Severe infectious complications were pneumonia (5.3 % (2 of 38), 8.3 % (4 of 48), 21.7 % (5 of 23) and 55.9 % (19 of 34) of persons in ІВ, ІІВ, ІС and ІІС groups, respectively) and spontaneous bacterial peritonitis (in 17.4 % (4 of 23) and 26.5 % (9 of 34) of patients of ІC and ІІC groups, respectively).
In all patients, SCE, LII, TNFα, hs-CRP and resistin levels increased with increasing decompensation of the disease (Table 2). In particular, in patients of group I with stage A, SCE was (39.48 ± 0.29) %, i.e. 1.44 times higher that of the control group; with stage B — (57.26 ± 0.42) %, which is 1.45 and 2.09 times higher than in the group of patients with stage A and in controls, respectively; with stage C — (86.13 ± 0.47) %, i.e. 2.18, 1.5 and 3.15 times higher than in the groups with stages A and B and in the control group, respectively. In patients of group II with stage A, SCE was (46.19 ± 0.38) % that is 1.69 times higher than in the control group; with stage B — (69.45 ± 0.44) %, which is 1.50 and 2.54 times higher than in the group of patients with stage A and in controls, respectively; with stage C — (93.71 ± 0.51) %, i.e. 2.03, 1.35 and 3.43 times higher than in the groups with stages A and B and in the control group, respectively. SCE was significantly higher in patients of groups ІІА, ІІВ and ІІС than in persons from IA, IB and IC groups (p < 0.05).
In persons of group I with stage A, LII parameters were 1.50 ± 0.09 that 2.54 times exceeded that of the control group; with stage B — 1.90 ± 0.15, which is 1.27 and 3.22 times higher than in the group of patients with stage A and in controls, respectively; with stage C — 2.50 ± 0.14, i.e. 1.67, 1.32 and 4.24 times higher than in patients with stage A, stage B and in control group, respectively. In patients of group II with stage A, LII parameters were 1.80 ± 0.08 that 3.05 times exceeded that of the control group; with stage B — 2.20 ± 0.13 that is 1.22 and 3.73 times higher than in the group of patients with stage A and in controls, respectively; with stage C — 2.70 ± 0.16, i.e. 1.50, 1.23 and 4.58 times higher than in the groups with stages A and B and in the control group, respectively. LII parameters were significantly higher in patients of IIA, ІІВ, and IIC groups than in individuals from IA, IB and IC groups (p < 0.05).
Hs-CRP level in patients of group I with stage A was (3.72 ± 0.10) mg/l, i.e. 5.72 times higher than that of the control group; with stage B — (7.24 ± 0.33) mg/l, which is 1.96 and 11.14 times higher than in the group of patients with stage A and in the control group, respectively; with stage C — (11.03 ± 0.75) mg/l, i.e. 2.97, 1.52 and 16.97 times higher than in the groups with stage A, stage B and in controls, respectively. In patients of group II with stage A, hs-CRP level was (5.85 ± 0.19) mg/l that was 9 times higher than in the control group; with stage B — (10.48 ± 0.42) mg/l, which is 1.79 and 16.12 times higher than in the group of patients with stage A and in the control group, respectively; with stage C — (15.71 ± 0.90) mg/l, i.e. 2.69, 1.50 and 24.17 times higher than in the groups with stages A and B and in the control group, respectively. Hs-CRP level was significantly higher in patients of groups IIA, IIB, and IIC than in persons from groups IA, IB and IC (p < 0.05).
TNFα in patients of group I with stage A was (40.59 ± 1.22) pg/ml and 2.34 times exceeded that of the control group; with stage B — (55.03 ± 2.46) pg/ml, which is 1.36 and 3.17 times higher than in the group of patients with stage A and in the control group, respectively; with stage C — (70.21 ± 3.14) pg/ml, i.e. 1.73, 1.28 and 4.04 times higher than in the groups with stage A and B and in controls, respectively. In patients of group II with stage A, TNFα level was (61.23 ± 2.75) pg/ml and 3.52 times exceeded that of the control group; with stage B — (84.39 ± 3.72) pg/ml, which is 1.38 and 4.86 times higher than in the group of patients with stage A and in the control group, respectively; with stage C — (102.58 ± 5.49) pg/ml, i.e. 1.67, 1.22 and 5.9 times higher than in the groups with stages A and B and in the control group, respectively. TNFα level was significantly higher in patients of groups IIA, IIB and IIC than in individuals from IA, IB and IC groups (p < 0.05).
The level of resistin in patients of group I with stage A was (4.23 ± 0.83) ng/ml and 1.14 times exceeded that of the control group; with stage B — (6.73 ± 0.21) ng/ml, which is 1.59 and 1.81 times higher than in the group of patients with stage A and in the control group, respectively; with stage C — (9.68 ± 0.47) ng/ml, i.e. 2.29, 1.44 and 2.60 times higher than in the groups with stage A, stage B and in controls, respectively. In patients of group II with stage A, the resistin level was (10.72 ± 0.82) ng/ml that is 2.88 times higher than that of the control group; with stage B — (13.74 ± 0.94) ng/ml, which is 1.28 and 3.69 times higher than in the group of patients with stage A and in the control group, respectively; with stage C — (15.96 ± 1.36) ng/ml, i.e. 1.49, 1.16 and 4.29 times higher than in the groups with stages A and B and in controls, respectively. Resistin levels were significantly higher in groups IIA, IIB and IIC than in IA, IB and IC groups (p < 0.05).
Patients suffering from alcoholic liver cirrhosis with concomitant NAFLD had the correlations between the level of resistin and the parameters of endogenous intoxication and immune-inflammatory process (Table 3) that indicates a direct connection of adipokine with such pathogenetic links of the disease.
Discussion
Patients with a combination of ALC and NAFLD had a more severe clinical picture with the development of astheno-vegetative, pain, dyspeptic, hepatorenal, hepatopulmonary syndromes, jaundice, portal hypertension, liver encephalopathy. Among the severe infectious complications, pneumonia and spontaneous bacterial peritonitis were more common in persons with subcompensation and decompensation.
The parameters of endogenous intoxication and immune-inflammatory process in patients with ALC associated with NAFLD and their changes depending on the stage of compensation have been studied. High levels of resistin in the blood serum of such patients were detected compared to the controls. These levels increased proportionally to the severity of LC. Thus, it can be concluded that an increase in the level of resistin is associated with a impaired liver function. Such data are consistent with the results of Kakizaki, Boutari et al. study, which demonstrated the independence of the resistin level from the etiological factor, but the dependence on the presence and progression of the immune-inflammatory process [16, 17]. This is due to the fact that apart from the adipose tissue, resistin is mainly produced by the blood mononuclear cells. Consequently, their activation increases resistin production. Confirming this view, Trzeciak-Ryczek et al. in their study noted that the stimulation of macrophages by lipopolysaccharide or proinflammatory cytokines (IL-1, IL-6 and TNFα) significantly increased resistin production in the infectious process [18].
Musso, Gambino et al. found a direct relationship between CRP and resistin level [19]. Kasztelan-Szczerbinska et al. confirmed the positive correlation of serum concentration of resistin with the level of leukocytes and CRP in patients with ALD [11]. Proinflammatory properties of resistin were also proved in other diseases. In particular, Kemmotsu et al. studied Kawasaki’s disease, Tanaka et al. — systemic autoimmune diseases, Yoshino and Su et al. — rheumatoid arthritis, Shen et al. — nonalcoholic steatohepatitis [20–24].
Positive correlations between resistin level and TNFα, hs-CRP, SCE, and LII were found. These results indicate the presence of resistin in immune-inflammatory processes and the development of endogenous intoxication in ALC. Higher levels of such parameters were observed in patients with ALC associated with NAFLD due to a more severe course of the pathological condition.
Conclusions
Analyzing the results of the study, it was found that with an increase in ALC decompensation, the degree of endogenous intoxication, which is accompanied by the development of immune-inflammatory response, is increasing, as evidenced by elevated SCE, LII, TNFα, hs-CRP and resistin levels.
Significantly higher SCE, LII and the content of TNFα, hs-CRP and resistin were detected in patients with a combination of ALC and NAFLD accompanied by a more severe course of the disease.
In patients with ALCs associated with NAFLD, correlation between the resistin level and SCE, LII, TNFα, hs-CRP was found.
Conflicts of interests. Authors declare the absence of any conflicts of interests that might be construed to influence the results or interpretation of their manuscript.
1. Allen A.M., Kim W.R. Epidemiology and healthcare burden of acute-on-chronic liver failure // Sem. Liv. Dis. 2016 May; 36(2): 123-6.
2. Bekaert M., Verhelst X., Geerts A., Lapauw B., Calders P. Association of recently described adipokines with liver histology in biopsy-proven non-alcoholic fatty liver disease: a systematic review // Obes. Rev. 2016 Jan; 17(1): 68-80. doi: 10.1111/obr.12333.
3. Aller R., Burgueño Gomez B., Sigüenza R., Fernández-Rodríguez C., Fernández N., Antolín B. et al. Comparative study of overweight and obese patients with nonalcoholic fatty liver disease // Rev. Esp. Enferm. Dig. 2019 Apr; 111(4): 256-263. doi: 10.17235/reed.2019.5926/2018.
4. Fazel Y., Koenig A.B., Sayiner M. et al. Epidemiology and natural history of non-alcoholic fatty liver disease // Metabolism. 2016; 65(8): 1017-25. doi: 10.1016/j.metabol.2016.01.012.
5. Kim D., Kim W.R. Nonobese fatty liver disease // Clin. Gastroenterol. Hepatol. 2017; 15(4): 474-85. doi: 10.1016/j.cgh.2016.08.028.
6. Coelho M., Oliveira T., Fernandes R. Biochemistry of adipose tissue: an endocrine organ // Archives of Medical Science. 2013; 9(2): 191-200. doi: 10.5114/aoms.2013.33181.
7. Panera N., Della Corte C., Crudele A., Stronati L., Nobili V., Alisi A. Recent advances in understanding the role of adipocytokines during non-alcoholic fatty liver disease pathogenesis and their link with hepatokines // Expert Rev. Gastroenterol. Hepatol. 2016; 10(3): 393-403. doi: 10.1586/17474124.2016.1110485.
8. Zhang Q., Wang Y., Liu Y., Yang Q., Wang X. et al. Effects of telmisartan on resistin expression in a rat model of nonalcoholic steatohepatitis and insulin resistance // Zhonghua Gan. Zang. Bing. Za Zhi. 2015 Apr; 23(4): 281-5. doi: 10.3760/cma.j.issn.1007-3418.2015.04.010.
9. Bedossa P. Pathology of non-alcoholic fatty liver disease // Liver Int. 2017; 37(Suppl. 1): 85-9. doi: 10.1111/liv.13301.
10. Garbuzenko D., Arefyev N., Kazachkov E. Antiangiogenic therapy for portal hypertension in liver cirrhosis: Current progress and perspectives // World J. Gastroenterol. 2018; 24(33): 3738-3748.
11. Kasztelan-Szczerbinska B., Surdacka A., Slomka M., Rolinski J., Celinski K., Smolen A. et al. Association of serum adiponectin, leptin, and resistin concentrations with the severity of liver dysfunction and the disease complications in alcoholic liver disease // Mediators of Inflammation. 2013, Oct 23; 2013: 1-12. doi: 10.1155/2013/148526.
12. Ayeser T., Basak M., Arslan K., Sayan I. Investigating the correlation of the number of diagnostic criteria to serum adiponectin, leptin, resistin, TNF-alpha, EGFR levels and abdominal adipose tissue // Diabetes Metab. Syndr. 2016 Apr-Jun; 10(2, Suppl. 1): 165-9. doi: 10.1016/j.dsx.2016.03.010.
13. Fukui H., Saito H., Ueno Y., Uto H., Obara K., Sakaida I. et al. Evidence-based clinical practice guidelines for liver cirrhosis 2015 // J. Gastroenterol. 2016; 51: 629-650.
14. Hadizadeh F., Faghihimani E., Adibi P. Nonalcoholic fatty liver disease: diagnostic biomarkers // World J. Gastrointest. Pathophysiol. 2017; 8(2): 11-26. doi: 10.4291/wjgp.v8.i2.11.
15. European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD) and European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease // Journal of Hepatology. 2016; 64: 1388-1402.
16. Kakizaki S., Sohara N., Yamazaki Y., Horiguchi N., Kanda D., Kabeya K. et al. Elevated plasma resistin concentrations in patients with liver cirrhosis // Journal of Gastroenterology and Hepatology. 2006; 23 (2008): 73-77. doi:10.1111/j.1440-1746.2006.04757.x.
17. Boutari C., Perakakis N., Mantzoros C.S. Association of adipokines with development and progression of nonalcoholic fatty liver disease // Endocrinol. Metab. (Seoul). 2018 Mar; 33(1): 33-43. doi: 10.3803/EnM.2018.33.1.33.
18. Trzeciak-Ryczek A., Tokarz-Deptuła B., Deptuła W. Adipocytokines affecting the immune system — selected data // Central European Journal of Immunology. 2011; 36(2): 92-94.
19. Musso G., Cassader M., De Michieli F., Paschetta E., Pinach S., Gambino R. et al. MERTK rs4374383 variant predicts incident nonalcoholic fatty liver disease and diabetes: role of mononuclear cell activation and adipokine response to dietary fat // Hum. Mol. Genet. 2017, May 1; 26(9): 1747-1758. doi: 10.1093/hmg/ddw400.
20. Kemmotsu Y., Saji T., Kusunoki N., Tanaka N., Nishimura C., Ishiguro A., Kawai S. Serum adipokine profiles in Kawasaki disease // Mod. Rheumatol. 2012; 22: 66-72. doi: 10.3109/s10165-011-0468-x.
21. Tanaka N., Masuoka S., Kusunoki N., Nanki T., Kawai S. Serum resistin level and progression of atherosclerosis during glucocorticoid therapy for systemic autoimmune diseases // Metabolites. 2016 Sep; 6(3): 28. doi: 10.3390/metabo6030028.
22. Yoshino T., Kusunoki N., Tanaka N., Kaneko K., Kusunoki Y., Endo H. Elevated serum levels of resistin, leptin, and adiponectin are associated with C-reactive protein and also other clinical conditions in rheumatoid arthritis // Intern. Med. 2011; 50(4): 269-75.
23. Su C.M., Huang C.Y., Tang C.H. Characteristics of resistin in rheumatoid arthritis angiogenesis // Biomark. Med. 2016 Jun; 10(6): 651-60. doi: 10.2217/bmm.15.125.
24. Shen Ch., Zhao C.Y., Wang W., Wang Y.D., Sun H., Cao W. et al. The relationship between hepatic resistin overexpression and inflammation in patients with nonalcoholic steatohepatitis // BMC Gastroenterology. 2014; 14: 39. doi: 10.1186/1471-230X-14-39.

/26-1.jpg)
/27-1.jpg)