Журнал «Здоровье ребенка» Том 14, №4, 2019
Вернуться к номеру
Cироваткові концентрації нейротрансмітерів у дітей iз рекурентними інфекціями верхніх дихальних шляхів
Авторы: L.S. Ovcharenko, D.M. Sheludko, A.O. Vertehel, I.V. Samokhin, T.G. Andrienko, A.V. Kryazhev
State Institution “Zaporizhzhia Medical Academy of Postgraduate Education of the Ministry of Health of Ukraine”, Zaporizhzhia, Ukraine
Рубрики: Педиатрия/Неонатология
Разделы: Клинические исследования
Версия для печати
Актуальність. Діти молодшого шкільного віку схильні до частих захворювань органів дихання. У структурі загальної захворюваності ця патологія посідає перше місце. Її поширеність становить понад 60 %, що призводить до частих пропусків школи, відсутності активних ігор і прогулянок на свіжому повітрі. Зважаючи на це збільшується кількість часу, який дитина витрачає на засоби масової електронної комунікації і електронні ігри, що призводить до високої прихильності, навiть до залежності, формуючи гіподинамію та підвищення психоемоційного напруження, що в сукупності має негативний вплив на функціонування регуляторних систем дитячого організму. Рекурентні інфекції верхніх дихальних шляхів (ІВДШ) викликають напруження нейроендокринно-імунної регуляції, що призводить до дисбалансу нейропептидів — медіаторів нейрогенного запалення. Метою цiєї роботи є вивчення показників нейрогенного запалення у школярів молодших класів iз рекурентною патологією респіраторного тракту. Матеріали та методи. Ми обстежили 130 дітей iз рекурентними ІВДШ віком від 6 до 9 років у період соматичного благополуччя. Проведено аналіз умісту вазоактивного інтестинального пептиду (ВІП), субстанції Р і кінцевих стабільних метаболітів оксиду азоту (КСМ NO) у сироватці крові. Виявлено підвищення рівня субстанції Р у школярів iз рекурентними ІВДШ, що мало статистично вірогідні відмінності iз показниками умовно здорових дітей (р < 0,05). Результати. Установлено, що за високих концентрацій субстанції Р підвищується ризик розвитку повторних захворювань. Доведено, що в дітей iз рекурентними ІВДШ за рахунок підвищення сироваткового вмісту КСМ NO, які мають прозапальну спрямованість, посилюється активність нейрогенного запалення. Виявлено, що при вірогідному зниженні вмісту ВІП як протизапального трансмітера в дітей iз рекурентними ІВДШ неможливе пригнічення активності нейрогенного запалення, що призводить до його надмірної стимуляції. Висновки. Діти з рекурентними ІВДШ у період соматичного благополуччя мають підвищені концентрації субстанції Р і КСМ NO в плазмі крові. У період соматичного благополуччя в дітей раннього шкільного віку з рекурентними ІВДШ спостерігається зниження рівня протизапального нейропептиду ВІП.
Актуальность. Дети младшего школьного возраста подвержены частым заболеваниям органов дыхания. В структуре общей заболеваемости данная патология занимает первое место. Ее распространенность составляет более 60 %, что приводит к частым пропускам школы, отсутствию активных игр и прогулок на свежем воздухе. Ввиду этого увеличивается количество времени, которое ребенок тратит на средства массовой электронной коммуникации и электронные игры, что приводит к высокой привязанности, вплоть до зависимости, формируя гиподинамию и повышение психоэмоционального напряжения, что в совокупности оказывает негативное влияние на функционирование регуляторных систем детского организма. Рекуррентные инфекции верхних дыхательных путей (ИВДП) вызывают напряжение нейроэндокринно-иммунной регуляции, что приводит к дисбалансу нейропептидов — медиаторов нейрогенного воспаления. Целью данной работы является изучение показателей нейрогенного воспаления у школьников младших классов с рекуррентной патологией респираторного тракта. Материалы и методы. Мы обследовали 130 детей с рекуррентными ИВДП в возрасте от 6 до 9 лет в период соматического благополучия. Проведен анализ содержания вазоактивного интестинального пептида (ВИП), субстанции Р и конечных стабильных метаболитов оксида азота (КСМ NO) в сыворотке крови. Выявлено повышение уровня субстанции Р у школьников с рекуррентными ИВДП, которое имело статистически достоверные различия с показателями условно здоровых детей (р < 0,05). Результаты. Установлено, что при высоких концентрациях субстанции Р повышается риск развития повторных заболеваний. Доказано, что у детей с рекуррентными ИВДП за счет повышения сывороточного содержания КСМ NO, имеющих провоспалительную направленность, усиливается активность нейрогенного воспаления. Выявлено, что при достоверном снижении уровня ВИП как противовоспалительного трансмиттера у детей с рекуррентными ИВДП невозможно подавление активности нейрогенного воспаления, что приводит к его чрезмерной стимуляции. Выводы. Дети с рекуррентными ИВДП в период соматического благополучия имеют повышенные концентрации субстанции Р и КСМ NO в плазме крови. В период соматического благополучия у детей раннего школьного возраста с рекуррентными ИВДП наблюдается снижение уровня противовоспалительного нейропептида ВИП.
Background. Schoolchildren are prone to frequent respiratory tract diseases. In the structure of general morbidity, this pathology ranks first. Its prevalence is more than 60 %, which leads to frequent school absenteeism, lack of active games and outdoor walks. So, there is an increase in the amount of time that a child spent on means of mass electronic communication and electronic games, resulting in high affection and addiction, forming hypodynamia, which in aggregate has a negative impact on the regulatory systems functioning. Recurrent upper respiratory tract infections (URTI) contribute to the strain of neuro-endocrine-immune regulation, causing an imbalance of neuropeptides — mediators of neurogenic inflammation. The purpose of this work is to study the neurogenic inflammation parameters in schoolchildren with functional disorders of the cardiovascular system and recurrent respiratory tract diseases. Materials and methods. We surveyed 130 children with URTI aged 6 to 9 years in the somatic well-being period. The analysis of the contents of vasoactive intestinal peptide (VIP), substance P and final stable metabolites of nitric oxide (FSM NO) in serum was carried out. An increase in substance P level in children with recurrent URTI was found, which had statistically significant differences with the healthy children indices (p < 0.05). Results. It has been found that high concentration of substance P increases the risk of recurrent URTI. It has been proved that in children with recurrent URTI due to increased FSM NO serum content that has a pro-inflammatory orientation, there is an increased neurogenic inflammation activity. It was found that the reliable reduction in the content of VIP as an anti-inflammatory transmitter in children with recurrent URTI can not suppress the activity of neurogenic inflammation, resulting in its excessive stimulation. Conclusions. Children with recurrent URTI in the somatic well-being period have increased serum levels of substance Р and FSM NO. In the somatic well-being period in schoolchildren with recurrent URTI, a decrease in the concentration of anti-inflammatory neuropeptide VIP is observed.
діти; нейропептиди; субстанція Р; рекурентні інфекції верхніх дихальних шляхів
дети; нейропептиды; субстанция Р; рекуррентные инфекции верхних дыхательных путей
children; neuropeptides; substance Р; recurrent upper respiratory tract infections
Introduction
The human nervous and endocrine systems are controlled by adaptive homeostasis functioning. The nervous system influence is realized in the tissues through cell cholinergic and adrenergic receptors by altering the activity of the endocrine glands, as well as by the formation of active protein molecules — neuropeptides [8]. It is known that the inflammatory reaction pathogenesis goes beyond the immune mechanisms and involves neuronal interactions. This is due to the ability of immune cells stimulated by inflammation to produce neuropeptides similar to those produced in the central nervous system [11]. Neuroendocrine cells of the brain and immune cells are in close co-operation and exhibit signs of similarity in their organization [3, 8].
Among neuropeptides, we can identify those with anti-inflammatory (vasointestinal peptide (VIP)) and proinflammatory (substance P) effects [1, 5, 6]. VIP is produced by neurons, endocrine and immune cells and is present in most organs, including the central nervous system, heart, lungs, thyroid gland, kidneys, urinary and gastrointestinal tract, genital organs and immune system [2, 7]. VIP suppresses the expression of other inflammatory mediators [5]. Recent studies have shown that VIP operates directly on the mucosal immune system, where increases IgA synthesis, indica–ting the critical role of this peptide in inducing oral intole–rance [5].
Substance P is a peptide consisting of 11 amino acids that regulates the mucosal immune balance and chronic inflammation activity [11]. It is produced by macrophages, T-cells, dendritic cells and eosinophils. The production of substance Р by macrophages induces bacterial lipopolysaccharides [14]. Substance P is currently considered as the main neurogenic inflammatory mediator capable of causing pathophysiological reactions such as edema, mucus hypersecretion, bronchospasm, vascular tone reduction, increased permeability of postcapillary venules, immune cell penetration into the tissues and secreting glands, enhancing monocyte/macrophags chemotaxis, control of T1 response, increasing the production of interferon g [14], proinflammatory activity and secretion of tumor necrosis factor a, interleukins 1, 6, 8, 12 [9].
Another substance that has proinflammatory properties is nitric oxide (NO) — a biological messenger molecule synthesized from the amino acid L-arginine in endothelial cells, macrophages, and neurons. NO mediates a wide range of important biological processes such as vasodilation, platelet aggregation inhibition, inflammation, immunoregulation and information transmission between the central nervous system neurons and the peripheral nervous system [4, 13, 14]. NO stimulates perivascular neurogenic inflammation by facilitating the synthesis and release of immunoreactive neurotransmitters such as substance P from nociceptive afferent fibers [4]. Increasing the NO concentration in children is observed in conditions accompanied by a change in the cytokine activity — acute infection, bronchopulmonary chronic diseases, persistent intracellular infection. NO concentration in exhaled air in children correlates with neutrophilia [11]. Indirect cytotoxic effect of NO is realized due to the action of free radical derivatives — peroxynitrite, nitrogen dioxide, hydroxyl radical, which initiate lipid peroxidation. NO metabolites — nitrates and nitrites — play an important role in the inflammation [14].
Given the role of neuropeptides in the immune response [11, 14], it is important to determine the effect of these mechanisms on the initial vegetative tone status in schoolchildren with upper respiratory tract infections (URTI). The possible neuroimmune mechanism disorders, as well as the hypodynamia effects, due to frequent exemptions from physical education classes, the prohibition of sports sections attending, and functional disorders of the cardiovascular system are the risk factors of cardiac organic pathology [3].
The purpose was to study neurogenic inflammation parameters in schoolchildren with functional disorders of the cardiovascular system and recurrent respiratory di–seases.
Materials and methods
One hundred and thirty children aged 6 to 9 years were examined. The analysis of the serum VIP, substance P and the biologically active substance — NO in the form of final stable metabolites (FSM NO) was carried out.
During the observation, children were divided into three groups: group 1 — those with functional disorders of the cardiovascular system and recurrent URTI (n = 50); group 2 — patients with functional disorders of the cardiovascular system and episodic URTI (n = 50); group 3 (controls) — conditionally healthy children (n = 30).
The study of serum FSM NO (nitrates, nitrites) was carried out by restoring nitrates to nitrites with the determination of the latter in reaction with the Griess reagent. The optical length was measured on spectrophotometer at a wavelength of 540 nm. Calculation of nitrite amount was carried out according to the calibration graph built on nitrogen. A quantitative determination of serum substance P and VIP was carried out by the immunoassay on Sunrise photometry analyzer (TECAN, Austria) using the ELISA kits (Peninsula Laboratories, LLC, San Carlos, USA).
The study uses statistical methods for information processing obtained: Fischer’s angle criterion, mean (M), mean error (m), Student’s t-test, Mann-Whitney U-test. ROC analysis of diagnostic tests was performed based on calculating the predictive value of the area under the ROC curve (AUC) with a cut-off point calculation.
Results
The examination of schoolchildren was carried out du–ring the period of somatic well-being. The results of the study are presented in Table 1.
When determining serum levels of substance P, VIP, FSM NO in group 1 children in the period of somatic well-being, there was a statistically significant (compared to group 3) increase in substance P concentration, FSM NO and a decrease in VIP content (p < 0.05). At the same time, a decrease in the serum VIP was noted compared to study group 2 (p < 0.05).
Analyzing the levels of substance P in children with recurrent and episodic URTI, one can conclude that no significant difference was found (U = 1071.0; p > 0.05), this is confirmed by the data of ROC analysis (Fig. 1).
ROC analysis of substance P serum concentration distribution between the 1 and 2 observation groups showed that the cut-off point was 0.31 ng/ml. Higher levels of substance P are associated with an increased risk of recurrent URTI. The optimal cut-off point is 0.31 ng/ml (AUC 0.6) with sensitivity of 26.0 % and specificity of 90.0 % (Fig. 1).
Among children with recurrent URTI and control group, there is a statistically significant difference in the concentration of substance P (U = 529.5; p < 0.05). Also, these differences in results are confirmed by data from ROC analysis (Fig. 2). ROC analysis of the distribution of substance P content in groups 1 and 3 showed that cut-off point is 0.3 ng/ml. Higher levels of substance R are associated with an increased risk of recurrent URTI. The optimal cut-off point is 0.3 ng/ml (AUC 0.7) with sensitivity of 33.0 % and specificity of 100.0 % (Fig. 2).
Determination of serum VIP in children of groups 1 and 2 showed significant differences, as evidenced by data of ROC analysis (Fig. 3).
Cut-off point for the serum concentration of VIP was determined, which corresponds to the level of 0.34 ng/ml. Lower levels are associated with an increased risk of recurrent URTI (AUC 0.8) with sensitivity of 68.0 % and specificity of 100.0 %. Similar results are obtained when comparing groups 1 and 3. The differences are also confirmed by ROC analysis data (Fig. 4). The cut-off point for VIP serum concentration is 0.28 ng/ml. VIP indices below this index will be associated with the risk of developing recurrent URTI (AUC 0.8) with sensitivity of 100.0 % and specificity of 50.0 %.
The determination of FSM NO serum content showed a slight difference between groups 1 and 2 (U = 873.0; p > 0.05) and the reliable differences between groups 1 and 3 (U = 377.5; p < 0.05). The conducted ROC analysis determined the cut-off point for FSM NO in the comparison groups 1 and 2 — 18.11 ng/ml. Serum concentration of FSM NO above this indicator was associated with an increased risk of recurrent URTI (AUC 0.7) with sensitivity of 44.0 % and specificity of 90.0 % (Fig. 5).
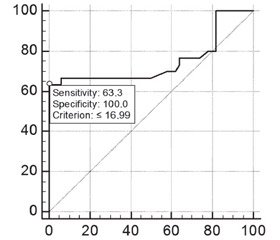
When comparing the indicators in groups 1 and 3, the serum level of FSM NO was 16.99 ng/ml by the cut-off point. Excess of this concentration is associated with a high risk of recurrent URTI (AUC 0.75) with sensitivity of 63.0 % and specificity of 100.0 % (Fig. 6).
Discussion
The inflammation pathogenesis goes beyond the scope of immune mechanisms — neuronal interactions are involved in this process. This is due to the ability of immunocompetent cells stimulated by inflammation to produce neuropeptides similar to those produced in the central nervous system [5]. Some neuropeptides/neurotransmitters have anti-inflammatory properties — one of them is VIP, and proinflammatory properties such as substance P and NO [8, 10, 14].
Based on the current theory of neuro-endocrine-immune regulation, immune responses can be considered as components of neuroendocrine activity, and by themselves they are impossible without the cohesive participation of the nervous and endocrine systems. Humoral regulatory factors affecting both of these systems are involved in the implementation of neuroimmune interactions [12].
Recurrent URTI in schoolchildren has a negative effect on the functional status of respiratory, cardiovascular, central nervous systems, changing the mechanism of pathological process, which is clinically manifested by the delayed recovery. The need to study the serum levels of neurotransmitters in schoolchildren with recurrent URTI allowed us to determine the degree of participation of neuro-immune inflammation in the pathogenesis of the disease and to allocate a risk group for the development of recurrent respiratory tract diseases. A comparative analysis of the serum substance P in schoolchildren showed significant differences between group 1 and the control group (p < 0.05). Exceeded the established concentration of substance P increases the risk of recurrent diseases.
The proinflammatory orientation of FSM NO, especially in children of group 1, may increase the activity of neurogenic inflammation. Probably, this due to the fact that in children with recurrent URTI on the background of increased activity of immunocompetent cells as a result of prolonged viral-bacterial stimulation, the production of central nervous system transmitters increased in response to a stressful situation, which is linked with recurrent di–seases [12]. Exceeding established concentration of FSM NO increases the risk of recurrent URTI.
A significant decrease in the content of anti-inflammatory transmitters, in particular VIP, in children with recurrent URTI can not suppress the activity of neurogenic inflammation.
Conclusions
1. In schoolchildren aged 6 to 9 years with recurrent URTI in the somatic well-being period, there is an increase in the serum concentration of neuroimmune proinflammatory mediators — substance P and FSM NO.
2. The period of somatic well-being in schoolchildren aged 6 to 9 years with recurrent URTI is characterized by a decrease in the concentration of anti-inflammatory neuropeptide VIP.
3. ROC analysis is a mechanism for predicting the risk of recurrent URTI.
Conflicts of interests. Authors declare the absence of any conflicts of interests that might be construed to influence the results or interpretation of their manuscript.
1. Григорьева В.А., Мельникова И.М., Мизерницкий Ю.Л. Современные представления о роли нейроиммунных звеньев в патогенезе заболеваний органов дыхания. Российский вестник перинатологии и педиатрии. 2011. Т. 56. № 4. С. 36-40.
2. Казюкова Т.В., Коваль Г.С., Самсыгина Г.А. и др. Часто болеющие дети: современные возможности снижения респираторной заболеваемости. Педиатрия. 2012. Т. 91. № 5. С. 42-48.
3. Муквіч О.М., Омельченко Л.І. Профілактика гострих респіраторних інфекцій у дітей шкільного віку. Дитячий лікар. 2013. № 6(27). С. 65-70.
4. Овчаренко Л.С., Шамрай И.В., Вертегел А.А. Нейроиммунные механизмы генеза частых повторных эпизодов острых бронхитов у детей. Перинатология и педиатрия. 2013. № 3.
С. 118-125.
5. Овчаренко Л.С., Волошин М.А., Вертегел А.О. та ін. Нейро–імунокорекція у дітей iз рекурентними бронхітами та перинатальними порушеннями центральної нервової системи: Методичні рекомендації. Київ, 2015. 19 с.
6. Речкина Е.А. Часто болеющие дети и роль иммунокоррекции в их лечении. Астма та алергія. 2013. № 1. С. 44-47.
7. Урясьев О.М., Шаханов А.В. Роль полиморфизма синтаз оксида азота в формировании коморбидной патологии бронхиальной астмы и гипертонической болезни. Казанский медицинский журнал. 2017. Т. 98. № 2. С. 226-232.
8. Щорічна доповідь про стан здоров’я населення, санітарно-епідемічну ситуацію та результати діяльності системи охорони здоров’я України. 2015 рік / за ред. Шафранського В.В.; МОЗ України, ДУ «УІСД МОЗ України». Київ, 2016. 452 с.
9. Ang S-F, Moochhala SM, MacAry PA, et al. Hydrogen sulfide and neurogenic inflammation in polymicrobial sepsis: involvement of substance P and ERK-NF-kB. Shi S, ed. PLoS ONE. 2011;6(9):e24535.
10. Chandrasekharan B, Nezami BG, Srinivasan S. Emerging neuropeptide targets in inflammation: NPY and VIP. American Journal of Phy–siology-Gastrointestinal and Liver Physiology. 2013;304(11):G949-G957. doi: 10.1152/ajpgi.00493.2012.
11. Ganea D, Hooper KM, Kong W. The neuropeptide VIP: direct effects on immune cells and involvement in inflammatory and autoimmune diseases. Acta physiologica (Oxford, England). 2015;213(2):442-452. doi: 10.1111/apha.12427.
12. Malhotra R. Understanding migraine: Potential role of neurogenic inflammation. Annals of Indian Academy of Neurology. 2016;19(2):175-182. doi: 10.4103/0972-2327.182302.
13. Souza-Moreira L, Campos-Salinas J, Caro M, et al. Neuropeptides as pleiotropic modulators of the immune response. Neuroendocrinology. 2011;94(2):89-100. doi: org/10.1159/000328636.
14. Waschek JA. VIP and PACAP: neuropeptide modulators of CNS inflammation, injury, and repair. British Journal of Pharmacology. 2013;169(3):512-523. doi: 10.1111/bph.12181.

/15-1.jpg)
/16-1.jpg)
/17-1.jpg)