Международный эндокринологический журнал Том 16, №3, 2020
Вернуться к номеру
Effect of vitamin D and B12 levels on hepatosteatosis in overweight and obese children
Авторы: Ayyıldız Civan H.(1), Papatya Çakır E.(1), Palabıyık F.(1), Cömert M.(2)
(1) — Bakırköy Dr. Sadi Konuk Training and Research Hospital, Istanbul, Turkey
(2) — Istambul Medipol University, Medicine Faculty, Istanbul, Turkey
Рубрики: Эндокринология
Разделы: Клинические исследования
Версия для печати
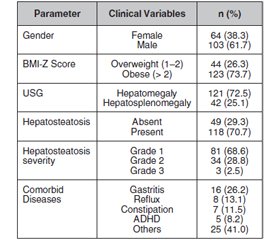
Актуальність. Неалкогольний стеатогепатоз у дітей призводить до зростання захворюваності та смертності в дорослому віці. Останнім часом опубліковані суперечливі дані стосовно взаємозв’язків між рівнями вітамінів D і B12 і частотою неалкогольного стеатогепатозу. Мета дослідження: оцінити зв’язок між рівнем вітамінів D і B12 та інсулінорезистентністю (ІР) і частотою неалкогольного стеатогепатозу в дітей з ожирінням та надмірною масою тіла. Матеріали та методи. У проспективне дослідження були включені 167 дітей із надмірною масою тіла та ожирінням віком від 5 до 18 років. Визначали антропометричні показники, включаючи масу тіла, зріст, індекс маси тіла (ІМТ) (вага/зріст2, кг/м2). У дітей і підлітків з ІМТ ≥ 95-го перцентиля для віку і статі діагностували ожиріння, а ІМТ від 85-го до 94-го перцентиля класифікували як надмірну масу тіла. Діти та підлітки були розподілені на дві групи: зі стеатогепатозом і без порушення функціонального стану печінки. Додатково оцінювали стан печінки за допомогою ультразвукового дослідження. Визначали демографічні характеристики учасників дослідження, проводили загальноклінічний огляд, лабораторні дослідження, включаючи аналізи на виявлення рівня вітаміну В12 і 25(OH)D у сироватці крові та визначення індексу ІР. Результати. Із 167 обстежених 103 (61,7 %) були чоловічої статі, 64 (38,3 %) — жіночої, їх середній вік становив 11,48 ± 2,99 року. Згідно з ІМТ у 26,3 % випадків була визначена надмірна маса тіла, а 73,7 % — ожиріння. Стеатогепатоз діагностований у 70,7 % випадків (n = 118), його частота була вірогідно вищою в пацієнтів чоловічої статі (79,6 %), ніж жіночої (p = 0,001). Середній показник ІР був статистично вищим у групі дітей зі стеатогепатозом (11,15 ± 13,39), ніж у контрольній групі (6,95 ± 6,20) (р = 0,029). Крім того, установлені статистично значущі відмінності рівнів ІР за ступенем вираженості стеатогепатозу (р = 0,013). Не спостерігалося вірогідного взаємозв’язку між дефіцитом вітамінів D та B12 і наявністю та тяжкістю стеатогепатозу (p > 0,05). Також не було виявлено статистично значущих відмінностей між середнім вмістом вітамінів D і В12 та індексом ІР серед дітей з ожирінням та надмірною масою тіла. Висновки. Отримані результати підтверджують опубліковані раніше дані про те, що дефіцит вітамінів D та B12 не сприяє розвитку стеатогепатозу в дітей із надмірною масою тіла та ожирінням. Інсулінорезистентність є фактором ризику виникнення та прогресування стеатогепатозу.
Актуальность. Неалкогольный стеатогепатоз у детей приводит к росту заболеваемости и смертности во взрослом возрасте. В последние годы опубликованы противоречивые данные о взаимосвязи между уровнями витаминов D и B12 и частотой неалкогольного стеатогепатоза. Цель исследования: оценить взаимосвязь между уровнем витаминов D и B12 и инсулинорезистентностью (ИР) и частотой неалкогольного стеатогепатоза у детей с ожирением и избыточной массой тела. Материалы и методы. В проспективное исследование были включены 167 детей с избыточной массой тела и ожирением в возрасте от 5 до 18 лет. Определяли антропометрические показатели, включая массу тела, рост, индекс массы тела (ИМТ) (вес/рост2, кг/м2). У детей и подростков с ИМТ ≥ 95-го перцентиля для возраста и пола диагностировали ожирение, а ИМТ от 85-го до 94-го перцентиля классифицировали как избыточную массу тела. Дети и подростки были разделены на две группы: со стеатогепатозом и без нарушения функционального состояния печени. Дополнительно оценивали состояние печени с помощью ультразвукового исследования. Определяли демографические характеристики участников исследования, проводили общеклинический обзор, лабораторные исследования, включая анализы на выявление уровня витамина В12 и 25(OH)D в сыворотке крови и определение индекса ИР. Результаты. Из 167 обследованных 103 (61,7 %) были мужского пола, 64 (38,3 %) — женского, их средний возраст составил 11,48 ± 2,99 года. Согласно ИМТ в 26,3 % случаев была выявлена избыточная масса тела, а в 73,7 % — ожирение. Стеатогепатоз диагностирован в 70,7 % случаев (n = 118), его частота была достоверно выше у пациентов мужского пола (79,6 %), чем женского (p = 0,001). Средний показатель ИР был статистически выше в группе детей со стеатогепатозом (11,15 ± 13,39), чем в контрольной группе (6,95 ± 6,20) (р = 0,029). Кроме того, установлены статистически значимые различия уровней ИР по степени выраженности стеатогепатоза (р = 0,013). Не наблюдалось достоверной взаимосвязи между дефицитом витаминов D и B12, наличием и тяжестью стеатогепатоза (p > 0,05). Также не было выявлено статистически значимых различий между средним содержанием витаминов D и В12 и индексом ИР среди детей с ожирением и избыточной массой тела. Выводы. Полученные результаты подтверждают опубликованные ранее данные о том, что дефицит витаминов D и B12 не способствует развитию стеатогепатоза у детей с избыточной массой тела и ожирением. Инсулинорезистентность является фактором риска возникновения и прогрессирования стеатогепатоза.
Background. The childhood non-alcoholic hepatosteatosis leads to significant morbidity and mortality in adulthood. In recent years, vitamin D and B12 deficiency has been controversially associated with non-alcoholic fatty liver disease. Therefore, we aimed to evaluate the relationship of vitamin levels and insulin resistance (IR) with non-alcoholic hepatosteatosis in obese and overweight children. Material and methods. A total of 167 overweight and obese children aged 5–18 years were enrolled in this prospective study. The anthropometric measurements including body weight, height, body mass index (BMI) (weight/height2, kg/m2) were recorded. Children and adolescents with ≥ 95th percentile of BMI for their age and gender were diagnosed with obesity, and BMI between the 85th and 94th percentiles was classified as overweight. Children and adolescents classified into two groups according to the presence of hepatosteatosis: normal liver and hepatosteatosis group. Additionally, hepatosteatosis grading was performed by ultrasonographic evaluation. Participants’ demographic characteristics, physical examination, imaging and laboratory findings including serum levels of vitamin B12, 25(OH)D analysis and insulin resistance index were documented and compared between groups. Results. One hundred and sixty-seven patients included in this study were: 103 (61.7 %) males, 64 (38.3 %) females, and the mean age of total participants was 11.48 ± 2.99 years. According to BMI-Z score, 26.3 % of individuals were defined as overweight and 73.7 % were obese. Hepatosteatosis was determined in 70.7 % (n = 118) of our cases and it was significantly higher in male patients (79.6 %) than in females (p = 0.001). Mean IR was statistically higher in non-alcoholic fatty liver disease group (11.15 ± 13.39) than in normal liver group (6.95 ± 6.20) (p = 0.029). Moreover, there were statistically significant differences found in IR levels according to severity of hepatosteatosis (p = 0.013). In addition, vitamin D and B12 deficiencies were not significantly associated with hepatosteatosis or severity of hepatosteatosis (p > 0.05). Also, no statistically significant differences were found in mean levels of vitamin D, vitamin B12 and IR between obese and overweight children. Conclusions. Our findings support the published data that vitamin D and B12 deficiencies do not contribute to the pathology of hepatosteatosis. In addition, insulin resistance has been demonstrated to be a risk factor for non-alcoholic fatty liver and hepatosteatosis severity.
стеатогепатоз; діти; ожиріння; дефіцит вітаміну В12; дефіцит вітаміну D; інсулінорезистентність
стеатогепатоз; дети; ожирение; дефицит витамина В12; дефицит витамина D; инсулинорезистентность
hepatosteatosis; non-alcoholic fatty liver disease; childhood obesity; vitamin B12 deficiency; vitamin D deficiency, insulin resistance
Introduction
Materials and methods
Results
Discussion
Conclusions
- Centers for Disease Control and Prevention. Childhood obesity causes & consequences. 2016. Retrieved from https://www.cdc.gov/obesity/childhood/causes.html.
- Bugianesi E., Bizzarri C., Rosso C., Mosca A. et al. Low birthweight increases the likelihood of severe steatosis in pediatric non-alcoholic fatty liver disease. The American Journal of Gastroenterology. 2017. 112(8). Р. 1277.
- Dowla S.A., Goss A.M., Ashraf A.P. Nonalcoholic Fatty Liver Disease in Children with Obesity. In Global Perspectives on Childhood Obesity. 2019. Р. 255-268.
- Rinella M.E. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015. 313(22). Р. 2263-73.
- Mahammad S.A., Nawaz S.S., Marx K.P., Siddiqu I.A. Relationship between serum vitamin B12, hyperhomocysteinemia in nonalcoholic fatty liver disease. International Journal of Bioassays. 2013. 2(11). Р. 1508-10.
- Baz-Hecht M., Goldfine A.B. The impact of vitamin D deficiency on diabetes and cardiovascular risk. Curr. Opin. Endocrinol. Diabetes Obes. 2010. 17. Р. 113-9.
- McGill A.T., Stewart J.M., Lithander F.E., Strik C.M., Poppitt S.D. Relationships of low serum vitamin D3 with anthropometry and markers of the metabolic syndrome and diabetes in overweight and obesity. Nutr. J. 2008. 7. Р. 4.
- Saberi B., Dadabhai A.S., Nanavati J., Wang L., Shinohara R.T., Mullin G.E. Vitamin D levels do not predict the stage of hepatic fibrosis in patients with non-alcoholic fatty liver disease: A PRISMA compliant systematic review and meta-analysis of pooled data. World Journal of Hepatology. 2018. 10(1). Р. 142.
- Wang X., Li W., Zhang Y., Yang Y., Qin G. Association between vitamin D and non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: results from a meta-analysis. Int. J. Clin. Exp. Med. 2015. 8. Р. 17221-17234.
- Koplay M., Gulcan E., Ozkan F. Association between serum vitamin B12 levels and the degree of steatosis in patients with nonalcoholic fatty liver disease. Journal of Investigative Medicine. 2011. 59(7). Р. 1137-1140.
- Nobili V., Giorgio V., Liccardo D., Bedogni G., Morino G., Alisi A., Cianfarani S. Vitamin D levels and liver histological alterations in children with nonalcoholic fatty liver disease. European Journal of Endocrinology. 2014. 170(4). Р. 547-53.
- Sezer O.B., Buluş D., Hızlı Ş., Andıran N., Yılmaz D., Ramadan S.U. Low 25-hydroxyvitamin D level is not an independent risk factor for hepatosteatosis in obese children. Journal of Pediatric Endocrinology and Metabolism. 2016. 29(7). Р. 783-788.
- Neyzi O., Bundak R., Gokcay G., Gunoz H., Furman A., Darendeliler F. et al. Reference values for weight, height, head circumference, and body mass index in Turkish Children. J. Clin. Res. Pediatr. Endocrinol. 2015. 7. Р. 280-293.
- Shannon A., Alkhouri N., Carter-Kent C., Monti L., Devito R., Lopez R., Feldstein A.E., Nobili V. Ultrasonographic quantitative estimation of hepatic steatosis in children with nonalcoholic fatty liver disease (NAFLD). Journal of Pediatric Gastroenterology and Nutrition. 2011. 53(2). Р. 190.
- Matthews D.R., Hosker J.P., Rudenski A.S., Naylor B.A., Treacher D.F., Turner R.C. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985. 28(7). Р. 412-419.
- Welsh J.A., Karpen S., Vos M.B. Increasing prevalence of nonalcoholic fatty liver disease among United States adolescents, 1988–1994 to 2007–2010. The Journal of Pediatrics. 2013. 162(3). Р. 496-500.
- Gordon C.M., DePeter K.C., Feldman H.A., Grace E., Emans S.J. Prevalence of vitamin D deficiency among healthy adolescents. Archives of Pediatrics & Adolescent Medicine. 2004. 158(6). Р. 531-537.
- Targher G., Bertolini L., Scala L., Cigolini M., Zenari L., Falezza G., Arcaro G. Associations between serum 25-hydroxyvitamin D3 concentrations and liver histology in patients with non-alcoholic fatty liver disease. Nutrition, Metabolism and Cardiovascular Diseases. 2007. 17(7). Р. 517-524.
- Wang X., Li W., Zhang Y., Yang Y., Qin G. Association between vitamin D and non-alcoholic fatty liver disease/non-alcoho–lic steatohepatitis: results from a meta-analysis. International Journal of Clinical and Experimental Medicine. 2015. 8(10). Р. 17221.
- Dursun F., Gerenli N., Dur S.M., Kirmizibekmez H. The relationship between vitamin D level and hepatosteatosis in obese children. Northern Clinics of Istanbul. 2018. 6(1). Р. 28.
- Katz K., Brar P.C., Parekh N., Liu Y.H., Weitzman M. Suspected nonalcoholic Fatty liver disease is not associated with vitamin d status in adolescents after adjustment for obesity. Journal of Obesity. 2011. 2010.
- Bolukbas F.F., İgnak S., Demirel O.U., Furuncuoglu Y., Mantar F., Sertel S.C., Saglam F.Y., Bolukbas C. Relationship between serum Vitamin B12 levels and hepatic fibrosis detected by transient elastography (Fibroscan) in non-alcoholic fatty liver disease. Anatol. Clin. 2017. 22(3). Р. 141-148.
- Polyzos S.A., Kountouras J., Patsiaoura K. et al. Serum vitamin B12 and folate levels in patients with non-alcoholic fatty liver disease. International journal of food sciences and nutrition. 2012. 63(6). Р. 659-666.
- Hirsch S., Poniachick J., Avendaño M., Csendes A., Burdiles P., Smok G., Diaz J.C., ía de la Maza M.P. Serum folate and homocysteine levels in obese females with non-alcoholic fatty liver. Nutrition. 2005. 21(2). Р. 137-141.
- Gaggini M., Morelli M., Buzzigoli E., DeFronzo R., Bugianesi E., Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013. 5(5). Р. 1544-1560.
- Fu J.F., Shi H.B., Liu L.R., Jiang P., Liang L., Wang C.L., Liu X.Y. Non-alcoholic fatty liver disease: an early mediator predicting metabolic syndrome in obese children? World Journal of Gastroenterology: WJG. 2011. 17(6). Р. 735.
- Tominaga K., Fujimoto E., Suzuki K., Hayashi M., Ichikawa M., Inaba Y. Prevalence of non-alcoholic fatty liver disease in children and relationship to metabolic syndrome, insulin resistance, and waist circumference. Environmental Health and Preventive Medicine. 2009. 14(2). Р. 142.
- Fraser A., Longnecker M.P., Lawlor D.A. Prevalence of elevated alanine aminotransferase among US adolescents and associated factors: NHANES 1999–2004. Gastroenterology. 2007. 133(6). Р. 1814-1820.

/42.jpg)
/43.jpg)