Международный эндокринологический журнал Том 16, №6, 2020
Вернуться к номеру
The association between obesity and thyroid stimulating hormone in adults
Авторы: Eyyüp Murat Efendioğlu(1), Duygu Kavuncuoğlu(2)
(1) — Gaziantep University, Department of Geriatrics, Gaziantep, Turkey
(2) — Hatay Health Directorate, Turkey
Рубрики: Эндокринология
Разделы: Клинические исследования
Версия для печати
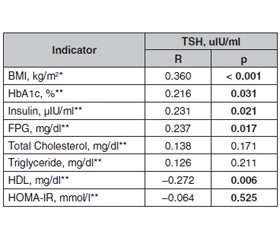
Актуальність. Ожиріння — найважливіша соціальна епідемія XXI століття. Особливо заслуговує на увагу часте поєднання патології щитоподібної залози (ЩЗ) та ожиріння. Ожиріння пов’язане з численними ендокринними патологіями, включаючи порушення функції ЩЗ та центральне ожиріння. Однак не встановлено, чи є розлад функції ЩЗ в осіб з ожирінням причиною цього стану чи його наслідком. Метою дослідження було з’ясувати взаємозв’язок між ожирінням та рівнем тиреотропного гормона (ТТГ) у плазмі крові. Матеріали та методи. Під спостереженням перебувало 73 пацієнти з ожирінням (індекс маси тіла (ІМТ) ≥ 30 кг/м2) віком 18–65 років та 27 осіб, які не страждають від ожиріння, з нормальним ІМТ. Реєстрували вік, стать, антропометричні вимірювання, рівень ТТГ, глюкози в плазмі натще (ГПН), інсуліну, загального холестерину, тригліцеридів та холестерину ліпопротеїдів високої щільності (ХС ЛПВЩ). Для аналізу даних використовували t-тест, U-тест Манна — Уїтні, критерій хі-квадрат та кореляційні тести Пірсона та Спірмена. Значення р < 0,05 вважали статистично значущим. Результати. У дослідження були включені 73 пацієнти з ІМТ ≥ 30 кг/м2 та 27 осіб, які не страждають від ожиріння. З числа обстежених було 59 жінок і 41 чоловік, середній вік яких становив 36,4 ± 10,4 року. Суттєві відмінності спостерігались у показниках ІМТ, ГПН, інсуліну, HbA1c, ХС ЛПВЩ та ТТГ між групами (р < 0,05). ТТГ вірогідно позитивно корелював із показниками ТТГ та ІМТ, HbA1c, інсуліну та ГПН у контрольній групі (p < 0,001, r = 0,360; p = 0,031, r = 0,231; p = 0,021, r = 0,231 і p = 0,017, r = 0,237 відповідно). Негативна кореляція відзначалася між ТТГ та ХС ЛПВЩ (p = 0,006, r = –0,272). Висновки. Значення ТТГ, глюкози в крові натще, HbA1c та інсуліну були вищими в групі з ожирінням порівняно зі здоровою групою з нормальною масою тіла, у той же час показники ХС ЛПВЩ були нижчими. Визначена вірогідна позитивна кореляція між ТТГ та ІМТ. Ці висновки підтверджують думку про те, що в осіб з ожирінням може спостерігатися незначне підвищення рівня ТТГ.
Актуальность. Ожирение — серьезная социальная эпидемия XXI века. Особого внимания заслуживает частое сочетание патологии щитовидной железы (ЩЖ) и ожирения. Ожирение связано с многочисленными эндокринными нарушениями, включая дисфункцию ЩЖ и центральное ожирение. Однако неясно, является ли заболевание ЩЖ у людей с ожирением причиной или следствием этого состояния. Целью исследования было выяснить взаимосвязь между ожирением и уровнем тиреотропного гормона (ТТГ) в плазме крови. Материалы и методы. Под наблюдением находились 73 пациента с ожирением (индекс массы тела (ИМТ) ≥ 30 кг/м2) в возрасте 18–65 лет и группа из 27 человек без ожирения с нормальным ИМТ. Ретроспективно регистрировали возраст, пол, антропометрические измерения, уровень ТТГ, глюкозы в плазме натощак (ГПН), инсулина, общего холестерина, триглицеридов и холестерина липопротеидов высокой плотности (ХС ЛПВП). Для анализа данных использовались t-критерий, U-критерий Манна — Уитни, критерий хи-квадрат и корреляционные тесты Пирсона и Спирмена. Значение p < 0,05 считалось статистически значимым. Результаты. В исследование были включены 73 пациента с ИМТ ≥ 30 кг/м2 и 27 лиц, которые не страдают от ожирения. Среди обследованных было 59 женщин и 41 мужчина, средний возраст которых составил 36,4 ± 10,4 года. Значительные различия наблюдались в значениях ИМТ, ГПН, инсулина, HbA1c, ХС ЛПВП и ТТГ между группами (p < 0,05). ТТГ достоверно положительно коррелировал с ТТГ и ИМТ, HbA1c, инсулином и ГПН (p < 0,001, r = 0,360; p = 0,031, r = 0,231; p = 0,021, r = 0,231 и p = 0,017, r = 0,237 соответственно). Отрицательная корреляция наблюдалась между ТТГ и ХС ЛПВП (p = 0,006, r = –0,272). Выводы. Значения ТТГ, глюкозы в крови натощак, HbA1c и инсулина были выше в группе с ожирением по сравнению с группой здоровых людей с нормальным весом, в то время как значения ХС ЛПВП были ниже. Определена достоверная положительная корреляция между ТТГ и ИМТ. Эти данные подтверждают мнение о том, что у людей с ожирением может наблюдаться небольшое повышение уровня ТТГ.
Background. Obesity is the most important social epidemic of the 21st century. The combination of increased thyroid pathology and obesity is particularly noteworthy. Obesity is associated with numerous endocrine abnormalities, including thyroid dysfunction and central obesity. However, it is unclear whether thyroid disorder in obese individuals is a cause of that condition or an effect. Obesity is the most important social epidemic of the 21st century. The combination of increased thyroid pathology and obesity is particularly noteworthy. Aim of the study was to elucidate the relationship between obesity and serum plasma thyroid stimulating hormone (TSH) level. Materials and methods. The records of 73 obese patients with BMI ≥ 30 kg/m2 among individuals aged 18–65 and a 27-member non-obese group with normal BMI were scanned retrospectively. Age, sex, anthropometric measurements, TSH, fasting plasma glucose (FPG), insulin, total cholesterol, triglyceride, and HDL results were recorded. The t test, Mann Whitney U test, chi square test, and Pearson and Spearman correlation tests were employed for data analysis. A p value < 0.05 was considered statistically significant. Results. Seventy-three patients with BMI ≥ 30 kg/m2 and 27 non-obese controls were included in the study. Fifty-nine of the individuals enrolled were women and 41 were men, with an average age of 36.4 ± 10.4 years. Significant differences were observed in BMI, FPG, insulin, HbA1c, HDL, and TSH values between the groups (p < 0.05). TSH was significantly positively correlated with TSH and BMI, HbA1c, insulin and FPG (p < 0.001, r = 0.360; p = 0.031, r = 0.231; p = 0.021, r = 0.231 and p = 0.017, r = 0.237, respectively). Negative correlation was present between TSH and HDL (p = 0.006, r = –0.272). Conclusions. TSH, fasting blood glucose, HbA1c and insulin values were higher in the obese group compared with the normal weight healthy group, while HDL values were lower. Significant positive correlation was determined between TSH and BMI. These findings support the idea that a slight increase in TSH levels may occur in obese individuals.
ожиріння; індекс маси тіла; тиреотропний гормон
ожирение; индекс массы тела; тиреотропный гормон
obesity; body mass index; thyroid stimulating hormone
Introduction
Material and methods
Results
/58_2.jpg)
Discussion
- http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed Mar 8, 2018.
- Nie X., Ma X., Xu Y., Shen Y., Wang Y., Bao Y. Characteristics of Serum Thyroid Hormones in Different Metabolic Phenotypes of Obesity. Front Endocrinol (Lausanne). 2020. 11. 68. doi: 10.3389/fendo.2020.00068.
- Biondi B. Thyroid and Obesity: An Intriguing Relationship. J. Clin. Endocrinol. Metab. 2010. 95(8). 3614-3617. https://doi.org/10.1210/jc.2010-1245.
- Biondi B., Cappola A.R., Cooper D.S. Subclinical Hypothyroidism: A Review. JAMA. 2019, Jul 9. 322(2). 153-160. doi: 10.1001/jama.2019.9052.
- Nyrnes A., Jorde R., Sundsfjord J. Serum TSH is positively associated with BMI. Int J Obes (Lond). 2006. 30. 100-5. doi: 10.1038/sj.ijo.0803112.
- Krotkiewski M. Thyroid hormones in the pathogenesis and treatment of obesity. Eur. J. Pharmacol. 2002. 440. 85-98. doi: 10.1016/s0014-2999(02)01420-6.
- Jee-Young Oh, Yeon-Ah Sung, Hye Jin Lee. Elevated thyroid stimulating hormone levels are associated with metabolic syndrome in euthyroid young women. Korean J. Intern. Med. 2013. 28. 180-6. doi: 10.3904/kjim.2013.28.2.180.
- Fontenelle L.C., Feitosa M.M., Severo J.S. et al. Thyroid function in human obesity: underlying mechanisms. Horm. Metab. Res. 2016. 48. 787-94. DOI: 10.1055/s-0042-121421.
- Lloyd R.V., Jin L., Tsumanuma I. et al. Leptin and leptin receptor in anterior pituitary function. Pituitary. 2001. 4. 33-47. https://doi.org/10.1023/A:1012982626401.
- Ortiga-Carvalho T.M., Oliveira K.J., Soares B.A., Pazos-Moura C.C. The role of leptin the regulation Of TSH secretion in the fed state: in vivo and in vitro studies. J. Endocrinol. 2002. 174. 121-5. doi: 10.1677/joe.0.1740121.
- World Health Organisation. Obesity: Preventing and managing the Global Epidemic. Report of a WHO Consultation on Obesity. Geneva. 1997. 3-5.
- Lacobellis G., Ribaudo M.C., Zappaterreno A. et al. Relation of thyroid function with body mass index, leptin, insulin sensitivity and adiponectin in euthyroid obese women. Clin. Endocrinol. 2005. 62. 487-91. https://doi.org/10.1111/j.1365-2265.2005.02247.x.
- Marzullo P., Minocci A., Tagliaferri M.A., Guzzaloni G., Di Blasio A., De Medici C. et al. Investigations of Thyroid Hormones and Antibodies in Obesity: Leptin Levels Are Associated with Thyroid Autoimmunity Independent of Bioanthropometric, Hormonal, and Weight-Related Determinants. Clin. Endocrinol. Metab. 2010. 95(8). 3965-72. doi: 10.1210/jc.2009-2798.
- Knudsen N., Laurberg P., Rasmussen L.B. et al. Small differences in thyroid function may be important for body mass index and the occurrence of obesity in the population. J. Clin. Endocrinol. Metab. 2005. 90. 4019-24. doi: 10.1210/jc.2004-2225.
- Douyon L., Schteingart D.E. Effect of obesity and starvation on thyroid hormone, growth hormone, and cortisol secretion. Endocrinol Metab. Clin. North. Am. 2002. 31(1). 173-89. doi: 10.1016/s0889-8529(01)00023-8.
- Zhang X., Li Y., Zhou X., Han X., Gao Y., Ji L. Association between serum thyrotropin within the euthyroid range and obesity. Endocr. J. 2019. 66. 451-457. doi: 10.1507/endocrj.EJ18-0140.
- Topsakal S., Yerlikaya E., Akin F., Kaptanoglu B., Erürker T. Relation with HOMA-IR and thyroid hormones in obese Turkish women with metabolic syndrome. Eat. Weight Disord. 2012. 17. 57-61. doi: 10.1007/BF03325329. PMID: 22751273.
- Garin M.C., Arnold A.M., Lee J.S., Tracy R.P., Cappola A.R. Subclinical hypothyroidism, weight change, and body composition in the elderly: the Cardiovascular Health Study. J. Clin. Endocrinol. Metab. 2014. 99(4). 1220-6. https://doi.org/10.1210/jc.2013-3591.
- Alkac C., Akbas F., Alkac B., Atmaca H.U. Obezitede tiroid fonksiyonları. JAREM. 2014. 2. 74-6. doi: 10.5152/ jarem.2014.466.
- Ekinci F., Merder-Coskun D., Tuncel B., Uzuner A. Obesity and thyroid function in adults Marmara Medical Journal. 2018. 31(2). 20-24. doi: 10.5472/marumj.430795

/58.jpg)