Резюме
Актуальність. Цукровий діабет (ЦД) асоціюється з підвищеною схильністю до інфікування, що частково пояснюється зниженою імунною відповіддю, опосередкованою Т-клітинами. Крім того, установлене порушення функції нейтрофілів, пов’язане з ЦД. Мета: визначити рівень обізнаності хворих на цукровий діабет 2-го типу стосовно імунізації проти гепатиту В, грипу, правця, а також з’ясувати джерело поточної інформації про вакцини. Матеріали та методи. Дослідження планувалось як проспективне, перехресне, описове та аналітичне. Анкета була застосована до пацієнтів із діагнозом ЦД 2-го типу, які звертались у лікарню, в амбулаторних умовах методом особистого опитування. Результати. Усього було опитано 439 пацієнтів. Розподіл пацієнтів за тривалістю ЦД такий: 38,5, 19, 24 та 18 % осіб — відповідно 0–5, 6–10, 11–15 років та більше 16 років. Ураження органів було виявлено в 76 пацієнтів, і як найбільш поширене ускладнення діагностована ретинопатія у 57 (13,01 %) пацієнтів. Серед пацієнтів у 175 осіб (39,86 %) була артеріальна гіпертензія, а 164 (37,36 %) із них мали супутню гіперліпідемію. 153 (35,75 %) пацієнти знали про пневмококову вакцину, кількість пацієнтів, які отримали щеплення, становила 55 (12,53 %). У той же час 336 (76,54 %) знали про вакцину проти грипу, 108 (24,60 %) із них отримали щеплення. Серед пацієнтів 179 (40,77 %) чули про вакцину проти гепатиту В, але лише 34 (7,74 %) отримали щеплення. Було встановлено, що 279 осіб чули про протиправцеву вакцину, 183 особам було введено принаймні одну дозу вакцини, проте останнє щеплення проводилося 101 (55,49 %) особі, які вакцинувалися проти правця понад 11 років тому. Лише 3 із 33 (7,52 %), які знали про інші вакцини, зробили щеплення. У цьому дослідженні 243 (55,35 %) людини отримали щеплення в зрілому віці з будь-якої причини. Не було значної залежності між рівнем освіти та тривалістю захворювання та вакцинацією. Висновки. Установлено, що рівень імунізації дорослих хворих на цукровий діабет є низьким. Фахівці первинної медичної допомоги відіграють важливу роль в імунізації хворих на цукровий діабет.
Background. Diabetes mellitus (DM) is associated with an increased rate of infection, which was partly explained by a decreased T cell-mediated response, and although being controversial, impaired function of neutrophil associated with diabetes is also documented. The purpose was to determine awareness of type 2 Diabetic patients about immunization against hepatitis-B, influenza, tetanus and zona, to find out the source of current vaccine information. Materials and methods. The study was planned as a single centred, prospective, cross-sectional, descriptive and analytical trial. The questionnaire form was applied to patients diagnosed with type 2 DM, who applied to Diabetics Outpatient Clinic by face-to-face interview technique. Results. A total of 439 patients was evaluated; the diagnosis time of 38.5, 19, 24 and 18 % of the patients was determined as 0–5 years, 6–10 years, 11–15 years and more than 16 years, respectively. Organ damage was detected in 76 of the patients, and as the most common complication, retinopathy was found to be in 57 (13.01 %) patients. Among the patients, 175 (39.86 %) of them had coexisting hypertension, and 164 (37.36 %) of them had coexisting hyperlipidaemia. Whereas 153 (35.75 %) were aware of pneumococcal vaccine, the number of patients who got vaccinated was 55 (12.53 %). Whereas 336 (76.54 %) were aware of influenza vaccine, 108 (24.60 %) of them got vaccinated. Among the patients, 179 (40.77 %) heard of hepatitis B vaccine, but 34 (7.74 %) got vaccinated. It was determined that, 279 people heard od tetanus vaccine, 183 people were administered at least one dose of vaccine, however the last vaccine of 101 (55.49 %) of those who had tetanus vaccine, was more than 11 years ago. Only 3 out of 33 (7.52 %), who knew about the zona vaccine, got vaccinated. In that study, 243 (55.35 %) people got vaccinated in adulthood for any reason. There was no significant relationship between education level and duration of disease and vaccination. Conclusions. Adult immunization rates of diabetic patients were found to be in low levels. The primary care professionals play an essential role in the immunization of diabetic patients.
Introduction
The treatment type 2 diabetes mellitus (DM) which is the most common form of the disease aims to prevent acute complications that might occur as a result of sudden fall or rise of blood sugar level, to protect from renal, retinal, neural, cardiac and vascular chronic sequelae that might be caused by the disease in the long term [1]. It is estimated that 8.8 % of the world’s population, or 425 million of adults aged 20–79, have DM. It is predicted that 629 million people will have DM by 2045 [2].
DM is associated with an increased rate of infection, which was partly explained by a decreased T cell-mediated response, and although being controversial, impaired function of neutrophil associated with diabetes is also documented [3].
There are two main purposes of the treatment of DM, one of which is to ensure blood sugar regulation and to reduce possible complications. Vaccines are administered to people to be immunized before they get a specific disease. It stimulates the defence mechanism in the body and enables the formation of antibodies specific to the disease agent [4].
People with DM are more likely to die or be hospitalized due to the influenza. Several observational studies have shown that hospitalizations and mortality are reduced during the epidemic in diabetic patients who have been vaccinated against the influenza, and the vaccine is effective [5]. Wound complications are likely to develop in diabetic patients. Therefore, tetanus vaccine is of particular importance. The risk of streptococcal pneumonia, duration of treatment, length of hospital stay, complications and mortality rates are of patients with diabetes are higher compared to the population. In addition, influenza vaccination is of particular importance to protect patients from prolonged influenza infections [5].
International authorities recommend influenza, hepatitis B and pneumococcal vaccines to be administered to all diabetic patients. Some guidelines recommend recombinant herpes zoster vaccine to be administered at intervals of 2–6 months for diabetic patients 50 years and older [1, 6, 7].
In order to reach current immunization programs, patients should be conscious and willing to be vaccinated. It is also possible to reduce treatment costs by vaccination.
This study aims to determine the awareness of type 2 Diabetic patients on hepatitis B, influenza, tetanus, zona and pneumococcal immunization.
Materials and methods
Ethics Committee Approval
This study was conducted with the approval of the Clinical Research Ethics Committee of Bağcılar Training and Research Hospital of the University of Health Sciences (SBU). (Date: 15.03.2019 and Approval No: 2019.03.2.04.28).
Characteristics of the Study
The study was planned as a single centered, prospective trial. 618 patients diagnosed with type 2 DM who applied to SBU Bagcilar Health Application and Research Centre (SUAM) Diabetes Outpatient Clinic between the dates 01.04.2019 and 01.07.2019 constituted the universe of the cross-sectional, descriptive and analytical study. The questionnaire form was applied to the patients using face-to-face interview technique. The sample size was calculated using simple random sampling method on the patients who applied to SBU Bagcilar SUAM Diabetes Outpatient Clinic in April, May and June 2019. 439 people who met the inclusion criteria were included in the study. Verbal and written consent was obtained from all individuals included in the study. The questionnaire consisted of 27 questions evaluating the sociodemographic characteristics of patients, attitudes, behaviours information about adult immunization.
Inclusion Criteria
Patients diagnosed with type 2 DM who applied to SBU Bagcilar Diabetes Outpatient Clinic, agreed to participate in the study with their consent, and patients over 18 years old were included in the study.
Exclusion Criteria
Patients who did not want to participate in the study and did not give their consent, who were not diagnosed with type 2 DM, patients under the age of 18. Pregnant patients were excluded.
Study Questionnaire
In the study form given to the patients; age, gender, height, weight, travel abroad, HbA1c duration of type 2 DM, current treatment method of the patient, whether they got vaccinated after the age of 18, vaccine awareness, the source of vaccine awareness, whether they got vaccinated ot not, the reason for not being vaccinated, whether they had the influenza in the year they got vaccinated against influenza, how many times they got vaccinated against tetanus, were questioned. The study form was created by the researcher. Educational status, history of pneumococcal, hepatitis B, tetanus, influenza and zona vaccines were questioned while creating the form and the relationship between sociodemographic characteristics and whether they got vaccinated, was examined. The entire study form is shown in ANNEX-1.
Statistical Analysis of Data
In this study, statistical analyses were carried out using the NCSS (Number Cruncher Statistical System) 2007 Statistical Software (Utah, USA) package program. In addition to descriptive statistical methods (mean, standard deviation, frequency and percentage distributions), Shapiro Wilk normality test was used to analyze the distribution of variables in the data analysis, the independent t-test was used to compare variables with normal distribution, and the chi-square test was used to analyze qualitative data. The results were evaluated at a significance level of p < 0.05.
Results
Sample calculation of the study indicated that minimum 392 people should be reached at a level of confidence of 95 % and margin of error of 3 %. 439 patients who met the inclusion criteria were included in the study and evaluated.
Socio-demographic data
243 (55.35 %) of the participants in the study were female. The mean age of the whole group was 55.57 ± 10.31 years, the mean age of males was 55.76 ± 10.00 years, the mean age of females was 55.42 ± 10.35 years. Body mass index (BMI) of males was found to be 29.21 ± 4.24 kg/m2, and BMI of females was found to be 31.69 ± 4.79 kg/m2 (table 1).
When evaluated based on educational status, 77 (17.54 %) people were literate, 300 (68.34 %) were primary school graduates, 39 (8.88 %) were high school graduates, while the total of college and university graduates was 23 (5.24 %). 178 (40.55 %) of the patients, 126 of whom were male, had a smoking history; mean of smoking was calculated as 26.60 ± 15.39 package/years in males; while it was calculated as 15.33 ± 9.58 package/years in females (table 2).
When the patients were evaluated based on the duration of DM, it was seen that 169 (38.5 %) of them were diagnosed less than 5 years ago, 82 (18.68 %) were diagnosed 6 to 10 years ago, 109 (24.83 %) were diagnosed 11 to 15 years ago, 79 (18 %) were diagnosed 16 years ago (table 3). Regarding the treatment method of the patients, it was seen that 230 (52.39 %) used only oral antidiabetic drugs (OAD), 197 (44.87 %) used OAD and insulin together, 11 (2.51 %) used only insulin (table 3).
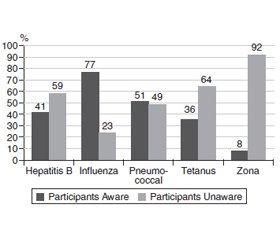
In the study conducted, 243 of the patients (55.35 %) were vaccinated at least once after the age of 18. Immunization awareness of the patients are shown in table 4 and fig. 1.
153 of the patients (35.75 %) knew the pneumococcal vaccine, while 275 (64.25 %) did not know the pneumococcal vaccine. The first source of information of those, who got vaccinated, were as follows; 20.26 % family physician, 30.72 % other specialist doctors, 2.61% other healthcare professionals, 29.41 % friends and family, 16.34% printed & visual media. Although 16 of 31 patients, who heard of the pneumococcal vaccine from their family physician and 35 of 47 patients, who heard of it from other specialist doctors, got vaccinated, 2 of 45 patients, who heard of it from friends/family got vaccinated and none of those, who heard it from printed and visual media got vaccinated. There is statistically significant difference between vaccination status of the patients, who heard of pneumococcal vaccine from their family physician, other specialist doctors and other healthcare professionals for the first time and those, who heard of it from other sources for the first time (p = 0.0001). 51.61 % of those, who heard of pneumococcal vaccine from their family physician and 74.47 % of those, who heard of it from other specialist doctors, got pneumococcal vaccine. Whereas 116 people stated that their reason for not being vaccinated was because it was not suggested by the doctor, the number of those, who consider vaccination unnecessary, was 18. The diagnosis periods of the patients were monitored in periods of 5 years. Accordingly, no statistically significant relationship was found between duration of diagnosis of patient with type 2 DM and whether pneumococcal vaccine was administered (p = 0.849).
136 (40.48 %) people heard of the influenza vaccine from printed & visual media, 101 (30.06 %) heard of it from their family physician, 33 heard of it from other healthcare professionals and 66 (19.64 %) heard of it from family/friends. 65 of 108 patients, who got vaccinated against the influenza, got vaccinated at family practice, 26 of them got vaccinated at a pharmacy. 76.36 % of the patients did not have the influenza during the flu season after being vaccinated against the influenza. 33.41 % of those, who got vaccinated against the influenza repeated vaccine every year, 7.41 % repeated every two years, 13.89% repeated every 3–5 years and 46.30 % repeated at a less frequency. A statistically significant difference was observed between the first source of information and the rate of vaccination of the influenza vaccine (p = 0.0001). The rate of vaccination of the patients, who were informed by their family physicians and other specialist doctors, was found to be high.
It was found that 260 (59.23 %) patients were not informed about the hepatitis B vaccine. 405 (92.26 %) of the patients did not have hepatitis B vaccine. 34 patients had hepatitis B vaccine. 15 (44.12 %) of those who got vaccinated, got vaccinated at family practice. The number of the patients who knew the hepatitis B vaccine but considered it unnecessary was 34 (7.74 %). 126 (31.34 %) of the patients stated that their reason for not being vaccinated was because it was not suggested by their doctor.
Although 183 patients were vaccinated against tetanus, 101 patients were vaccinated more than 11 years ago. Of those who were vaccinated against tetanus, 115 (62.84 %) were vaccinated after injury and 40 patients were vaccinated during pregnancy. 7 people who were vaccinated by their own will and 4 people who were vaccinated upon the doctor's recommendation were determined.
It was found that 406 (92.48 %) patients did not know about the zona vaccine. Source of information about zona vaccine was found to be as follows; 1 person heard of it from family physician, 8 from other specialist doctors, 12 from printed and visual media. It was determined what 3 people got vaccinated against zona, 1 of whom was vaccinated at Bağcılar Training and Research Hospital and 2 at a private hospital.
/18.jpg)
Immunization status of the patients are shown in table 5 and fig. 2. There is a statistically significant relationship between the increase in education level and the vaccination status after the age of 18 in the patients who participated in our study (p = 0.001). The vaccination of literate and high school graduate group was found to be low. There was no statistically significant relationship between education status and getting the influenza vaccine (p = 0.073). The rate of meningitis vaccination was found to be statistically lower in patients whose educational statues as literate (p = 0.006). No statistically significant difference was observed between pneumococcal vaccination of educational status groups after the age of 18 (p = 0.563). Hepatitis B vaccination rate was statistically lower in Literate and University groups (p = 0.019). A statistically significant difference was observed between the distribution of Tetanus diphtheria vaccine after the age of 18 in education groups (p = 0.0001).
/18_2.jpg)
Discussion
Vaccination is one of the most effective public health methods in preventing diseases. Although relatively good childhood vaccination is available in many parts of the world, the vaccine is not used in the prevention of diseases in adults or the adult vaccination rates are far below the targets [8]. In our study, the number of people, who had any vaccination in adulthood, among patients with type 2 DM, was found to be 243 (55.35 %). In order to achieve vaccination targets, guidelines and regulations prepared in accordance with current evidence-based guidelines should be prepared, regulations should be made with which vaccines can be administered, and vaccination campaigns should be planned.
Vaccination is still one of the most cost-effective methods in reducing morbidity and mortality associated with infectious diseases; however, challenges remain and persisting inequities in vaccine uptake contribute to the continued occurrence and outbreaks of vaccine-preventable diseases [9].
In a study conducted in Turkey to determine the immunization rates in adult patients with previous comorbidities, the mean age was found to be 40.03, the ones that were not vaccinated were found to be 72.8 %, the ones that were vaccinated were found to be 27.2 %, the rate of pneumococcal vaccination was found to be 1.0 %, the influenza vaccination was found to be 4.5 %, Hepatit B vaccination was found to be 4.1 %, Tetanus vaccination was found to be 22.8 % [10]. In another study conducted in 2015 with a participation of 318 individuals, information about the need for vaccination and the rates of vaccination of diabetic patients were found to be 34.5 to 15.5 % for Hepatitis B vaccine; 46 to 14.6 % for influenza vaccine; and 18.9 to 3.8 % for pneumococcal vaccine, respectively. In the same study, it was found that the most common source of information for patients was doctors with the rate of 71 % [11]. In a study conducted by Satman et al., effects of doctors on the influenza vaccination and pneumococcal vaccination were examined and it was shown that the rate of influenza vaccination of patients increased from 27 to 63.3 %, that of pneumococcal vaccination increased from 9,8% to 40.7% within one year after providing training to doctors on vaccines [12].
Pneumococcal vaccine is recommended in all current guidelines for diabetic patients [6–8]. 153 (35.75 %) of the patients in our study heard of the pneumococcal vaccine, however 55 (12.53 %) of them stated that they had the pneumococcal vaccine. None of 25 people who were informed about the pneumococcal vaccine through printed and visual media were vaccinated. Therefore, printed and visual media did not contribute to pneumococcal vaccination. 51% of the patients who were informed about the pneumococcal vaccine from their family physician and 74.47 % of the patients who were informed by other doctors were vaccinated. When vaccination rates were examined, it was found that the first source of information was healthcare professionals, compared to hearing of the vaccine from a source other than healthcare professionals. Therefore, doctors have a serious responsibility to create vaccine public opinion. 18 (4.10 %) patients were found to have heard of the vaccine but considered unnecessary. When asked the reason for not being vaccinated, 116 (26.4 %) patients stated that their doctor did not suggest it, while 217 (49.4 %) patients reported that they were unaware of the vaccine. A significant relationship was not found between the duration of diabetes and whether the patients had a pneumococcal vaccine.
It was seen that the influenza vaccination in diabetic patients reduced complications arising from the influenza by 56 %, hospitalizations by 54 % and deaths by 58 % [13]. Influenza vaccine reduces hospitalization and mortality in both the elderly and the elderly with DM, regardless of gender [14]. In our study, 336 of the patients (76.54 %) knew about the influenza vaccine. In the study conducted by Uzuner et al., similar to our study, the most known vaccine was found to be the influenza vaccine [15]. The 24.6 % vaccination rate in our study in the risk group is quite low. Although the primary source of the vaccine is mostly printed & visual media; when the vaccine is heard from the family physician and other specialist doctors, the rate of vaccination is higher. Only 13.24 % of the patients who got information from the printed and visual media were vaccinated. The vaccination rate of those whose source of information about the influenza vaccine is doctors, is higher, but the targeted vaccination rate cannot be achieved. Doctors and healthcare professionals should be pioneers in this issue. When we asked the patients whether they were sick in the flu season after being vaccinated against influenza, it was found out that 76.36 % of them did not get sick and were protected from seasonal flu. Only 35 (7.97 %) of the patients have made it a habit to be vaccinated every year. Reasons such as not considering the influenza as an important disease, not trusting in protection of vaccine, the vaccine causing some complaints, the thought of the vaccine causing the influenza, the pain the vaccinated area; reduce the rate of vaccination [16, 17].
In our study, although there were 179 (40 %) people who knew about hepatitis B vaccine, only 34 (7.74 %) of the patients were vaccinated. Considering the difficulty, chronicity and complications of hepatitis B treatment, it is recommended that diabetic patients under 60 should be vaccinated. Vaccination is recommended in diabetic patients over 60 years of age, even if the immune response is low [6–8].
In our study, 183 (41.69 %) of the patients were vaccinated against tetanus, but 101 patients did not get a tetanus vaccine for more than 11 years, so it can be thought that 55.49 % of those who got vaccinated, did not have a protective vaccine. While the vaccination process of 3 people continued, there were 46 people who got the last dose of vaccine within the last 0–5 years and 32 people within the last 6–10 years. 62.84 % of those vaccinated were vaccinated after an injury. 16.4 % of females were vaccinated during their pregnancy. There are 7 people who were vaccinated by their own will. The number of patients vaccinated in line with the doctor's recommendation is only 4. While 62.75 % of those who did not have a tetanus, vaccine stated that they did not know about the vaccine, 36.86 % thought that the tetanus vaccine was not necessary.
Recombinant zona vaccine is recommended for diabetic patients over 50 years of age with 2 doses at 2–6 months intervals [18]. The number of those who got zona vaccine od 439 patients, whose mean age was 55.5, was 3. There were 33 people who heard of the zona vaccine. However, 406 of our patients (92.48 %) had no information about the vaccine. According to a study conducted on 409 patients over 60 years of age, 29 % of the patients knew that the herpes zoster vaccine was recommended, 70 % of the patients had never heard of the vaccine, but 59% were interested in getting vaccinated after the questionnaire they filled out [19].
Although there are statistically significant differences between education level and getting vaccinated after the age of 18 depending on the vaccine, there was no consistent relationship between the increase or decrease in education level and immunization. The primary care professionals play an essential role in the immunization education [20].
Conclusions
The concept of adult immunization in preventive medicine and rational use of limited financial resources allocated to health in building a healthy society, was put forward by organizations such as World Health Organization. Our study revealed that adult immunization rates of diabetic patients were found to be in low levels. It is known that the frequency of infection, the need for hospitalization and death rates decreases with immunization of adults at risk for various infections.
Adult immunization record system can be formed starting from the risk groups and spreading to the whole population, free and easy access to these vaccines can be facilitated and the motivation of doctors for guidance can be increased.
There has always been some controversy surrounding vaccines, and people may have some concerns about safety immunization. Vaccines should continue to go through the most intensive safety monitoring. Patients with any questions about vaccines should first consult their primary health care providers for reliable information. As health consultants and educators, family physicians have important responsibilities in immunazation issues of diabetic patients that they follow.
Acknowledgement. The authors would like to thank all the participants.
Received 26.04.2021
Revised 25.05.2021
Accepted 04.06.2021

/17.jpg)
/18.jpg)
/18_2.jpg)