Introduction
The main goal in stroke rehabilitation is to prevent complications and maximize the present functions, so prepare individuals physically, mentally, socially and professionally. Preventing an event from repeating is another important goal [1]. Of the stroke patients, 20 % die in acute stage and in total 30 % die within a year; and one third of survivors continue their lives in need of others even in their daily works. These figures classify the stroke as illness causing morbidity and mortality most [2].
Early initiation of rehabilitation is vital for neurological deficits to recover as soon as possible with minimal damage. Rehabilitation should be maintained at home after the hospital discharge [3].
Preventing reoccurrence of stroke and providing patients and their families with appropriate care and skills are among nurses’ major duties [4]. In particular, care by specialized and educated nurses is necessary for patients newly diagnosed with stroke. The biggest support for patients to have the necessary information about this situation and cope with life change should be provided by nurses [5].
Providing consultancy and training is one of nurses’ major roles. Nurses should inform people about stroke symptoms, risk factors and current treatments.
Before discharge, patients should acquire physical and psychological knowledge and skills they need for their self care [6, 7]. Thus, discharge planning is necessary to prevent repeated applications, reduce healthcare costs and increase the quality of patient care [8]. The most important step during discharge is to determine the needs and provide appropriate training. Discharge training is a continuing and planned training that includes the process starting with the first day of hospitalization until the discharge and home care post discharge [9]. The planned discharge training shortens the duration of home care services, the level of anxiety and the repeated applications to the hospital. In contrast, it increases patient satisfaction [10].
Benefits of discharge training in terms of patients and the institution are as follows [11, 12]:
— It shortens hospitalization duration of patients.
— Home care is provided after the patient is discharged from hospital.
— Care quality of the patient increases.
— Satisfaction level of the patient and family increases.
— Patients are informed about the potential early or late complications and adapt more to the treatment.
— Knowledge and skills of the patients and caregivers regarding care increase.
— The patients develop self-confidence and leave for home more readily. They feel more precious during training as caregivers are also consulted and they become aware of where to consult and what they should do when they face problems.
In terms of the health institution [13, 14]:
— Repeated applications to the hospital decrease.
— As patients are satisfied, the institution is preferred more, thus, its quality standards increase.
— Health costs decrease.
Nurses have roles and responsibilities in discharge training such as planning the training of the patients and their family, informing them about care and treatment methods and possible side effects, providing patients with up-to-date and reliable health information. However, the studies conducted in Turkey have indicated that nurses do not provide training to patients and their families about discharge; the bed availability is not effectively used; and there is no a systematic discharge training to provide benefits to more patients. Patients and their families who do not receive effective discharge training go to hospital again as they face problems that they cannot resolve at home [14].
Risk factors of stroke disease
Stroke risk factors are divided into changeable and non-changeable risk factors. Unchangeable Risk Factors: Age, gender, race-ethnicity, family history. Changeable Risk Factors: Definite Risk Factors: Hypertension, Diabetes, Heart Diseases, Obesity, Dyslipidemia, Atrial Fibrillation, Asymptomatic Carotid Stenosis, Sickle Cell Anemia, Smoking. Undetermined Risk Factors: Alcoholism, Metabolic Syndrome, Sleep Respiratory Disorders, Migraine, Drug Addiction, Hypercoagulation [15].
Diabetes is Most Common Reason to Stroke Among Chronic Disaeses in Turkey
Diabetes is a chronic disease and its frequency is increasing both in the world and in our country. WHO refers to diabetes as an epidemic [16]. Diabetes complications impair the health of many of our organs. The increase in the incidence of diabetes is related to the increase in unhealthy diet, sedentary life and obesity. According to the IDF’s 2017 report. There are approximately 425 million people with diabetes in the world, which increases morbidity, mortality, as well as health costs.
According to IDF 9th Diabetes Atlas the number of people with diabetes in the 20–79 age group is estimated to be 629 million in 2045. The first 23 countries with the lowest diabetes prevalence in the age range 18–99 are African countries (Benin — 0.73 %, Zimbabve — 1 %, Uganda — 1.40 %), and when we look at developed countries, this rate is 9.99 % in Canada, 13.27 % in America, 10.54 % in New Zealand, 10.96 % in China. Is 8.19 % in Thailand, 7.84 % in Japan, 2.58 % in Greenland, 4.65 % in Ireland, 5.95 % in England [17]. Diabetes is on the rise all over the world.
The Turkey Diabetes Epidemiology Study (TURDEP-I) was conducted in 1997–1998 with the participation of 24.788 individuals in 540 centers across Turkey, and the prevalence of diabetes over 20 years of age was 7.2 % and impaired glucose tolerance was 6.7 %. According to TURDEP II in 2010, it was understood that the diabetes prevalence reached 13.7 %, moreover, the awareness of diabetes in the society decreased, and therefore, almost half of the diabetic people were previously undiagnosed and newly diabetic. In this study, prediabetes categories were also examined. The prevalence of impaired fasting glucose was 14.5 %, impaired glucose tolerance was 7.1 %, and combined glucose intolerance was 6.7 %. In the 9th Diabetes Atlas of IDF, it was determined that the diabetes prevalence of Turkey between the ages of 20–79 in 2017 was 12.8 %, IGT was 7.4 %, and diabetes health expenditures were 5.445 million dollars. In addition, the diabetes prevalence of our country between the ages of 18–99 is 12.54 %, and we are the 8th country with a high diabetes prevalence in Europe and 169th in the world. According to the estimates of IDF; It is predicted that by 2045 in Turkey, diabetes prevalence between the ages of 20–79 will be 16.5 %, IGT will be 8 %, and diabetes health expenditures will be 7,339 million dollars [17, 18].
Increasing rate of diabetes is related with unhealthy diet, sedentary lifestyle and increase in obesity. It is known that diabetes or its complications can be prevented or delayed by appropriate methods. For this reason, effective policies developed at national level should be implemented.
The purpose was to determine the learning needs and the factors affecting the need for discharge training in patients with stroke.
Materials and methods
The population of the study consisted of stroke patients who were hospitalized in the Neurology Service of a university hospital between April 15 and September 15, 2018. The stroke prevalence in the Turkish society is 254/100.000. The sample size of this study is 104 patients with 95 % reliability and 0.03 fault tolerence. A total of 120 patients participated in the study, yet 109 of them were included in the sample since 11 patients did not answer the whole questions.
Independent Variables of the Study: sociodemographic attributes and health & disease characteristics.
Dependent Variable: learning requirements scores.
Setting and Time Period of the Study: this study was conducted with patients, meeting the criteria and hospitalized in the Neurology Service of Health Sciences University Sultan Abdülhamid Han Training and Research Hospital between April 15 and September 15, 2018. This service includes Neurology Intensive Care, Neurology Clinic and the newly opened stroke center. There are 4 beds in the intensive care unit, 16 beds in the clinic and 4 beds in the stroke center to be opened. Twelve nurses work in the neurology service. Patients with stroke stay approximately 5 to 14 days in hospital.
Sampling Criteria:
— Aged over 18 years.
— Hospitalized by stroke.
— Conscious with full cooperation and orientation.
— Patients to be discharged and having 24–48 hours to be discharged.
Exclusion Criteria:
— Patients with aphasia and illiterate patients.
Data Collection Tools Used in the Research and Data Analysis
The data were collected through face-to-face interview with the participants. The data were obtained using the Introductory Information Form and and the Turkish version of the “Patient Learning Needs Scale (PLNS)” by the researchers. The PLNS was developed by N. Bubela et al. [19]. The scale consists of seven subscales (medications, activities of living, community and follow-up, feelings related to condition, treatment and complications, enhancing quality of life, and skin care) and a total of 50 items. Each item is scored on a Likert-type scale of 1 (not important) to 5 (extremely important). The total score ranges between 50 and 250. The Turkish validity and reliability study of the PLNS was conducted and found to be valid and reliable [20].
The data were analyzed using the PSPP and Microsoft Excel.
Research Ethics
Prior to the research, institutional permission from Health Sciences University Sultan Abdülhamid Han Training and Research Hospital, Ethics Committee Approval from Üsküdar University Non-Invasive Research Ethics Committee was obtained (B.08.6.YÖK.2.ÜS.0.05.0.06/2018/465). The Neurology Clinic Chief and Supervisor Nurse were informed. The patients provided voluntary informed consent form in written.
Results
The age of 109 participants ranged from 35 to 93, and the average was 67.38 ± 12.83; 62.4 % of the patients aged 65 years and over, 54.1 % were male, 36.7 % were primary school graduates, 64.2 % were married, 28.4 % were living with their spouse at home.
Of the patients, 84.4 % had a chronic disease, 77.1 % used drugs, 80.7 % did not smoke, 70.6 % had stroke only once, 49.5 % were in the hospital for 5 to 14 days, 55.0 % did not receive discharge training and 39.4 of 45.0 % of the patients who stated that they received discharge training received training from a nurse.
The difference in sub-dimensions of community, follow-up and skin care among the age groups was found to be statistically significant (p < 0.05). Learning needs of the patients aged 65 years and over increased more compared to those aged between 18 and 64 years from the community, follow-up and skin care sub-dimensions (table 1).
There was no statistically significant difference between the total scores from the learning needs scale and its sub-dimensions according to gender, education groups, marital status groups, presence of chronic disease and drug use knowledge (p > 0.05).
The treatment and complications sub-dimension was found to be statistically significant between the scores from learning needs total scale and its sub-dimensions according to the residential area (p < 0.05). Learning needs of the patients living with their spouses at home increased in the treatment and complications sub-dimension.
Sub-dimensions of medication, activities of living, community and follow-up, treatment and complications, skin care and total scale scores were found to be statistically significant according to smoking habits (p < 0.05). Patients who did not smoke had higher learning needs in the total scores and sub-dimensions (table 2).
There was no statistical significance in the number of strokes and the duration of hospitalization between the total scale score and sub-dimensions scores of learning needs (p > 0.05).
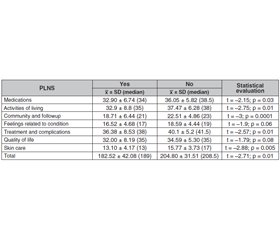
There was no statistical significance between the total scale score and sub-dimensions scores of learning needs according to discharge training (p > 0.05). There was statistical significance between the total scale score and sub-dimensions scores of learning needs according to the person having received discharge training (p < 0.05). The learning needs and total scores of all sub-dimensions of the patients who received discharge training from a nurse increased compared to the patients who received discharge training from a doctor (table 3).
Discussion
Patients need more information to adapt to their new health condition like stroke. Patient training helps patients to understand their diagnosis and treatment and to maintain their home care, to take part in self-care, to prevent potential complications of the disease, to take on their own health responsibility and to get rid of the feeling of inability and weakness due to their disease [21]. In particular, the training provided in the adaptation to the new situation is of great importance in complications after stroke which reduces their quality of life. In this sense, determining the patients’ learning needs should be prioritized. This study was conducted to determine the learning needs of patients with stroke and the factors affecting them. The data obtained were discussed in the light of the literature.
In this section, the distribution was analyzed over seven sub-dimensions and sum total upon the administration of PLNS to 109 participants. The total scale score was found to be 200.43 ± 34.77. The maximum obtainable score from the PLNS is 245 for this study. The 25th item was scored as 0 since it is not appropriate for this study. Some scores from the literature are as follows: 190.81 ± 17.05, 198.75 ± 30.60 for brain surgery patients, 201.73 ± 25.60 for surgical unit inpatients of a public hospital, 204.26 ± 23.88 for internal clinic inpatients, 203.65 ± 37.10 for women having undergone gynecological operation and 207.52 ± 24.14 for patients having undergone abdominal surgery, 199.6 ± 29.7 for patients having undergone colorectal cancer surgery, 175.82 ± 42.49 at the discharge phase of outpatient surgery patients, 186.67 ± 29.22 for inpatients in internal and surgical clinics, and 205.0 ± 26.7 for patients having a surgery [22].
The medication sub-dimension was found to be high at significance level in the sub-dimension mean score of 4.43. There are several studies having a sub-dimension with high significance level [22]. Unlike this study, there are studies with high significance levels in the sub-dimensions of treatment and complications [23].
Considering the mean score significance level of PLNS sub-dimension, the community and follow-up sub-dimension scored the lowest with 3.63. High learning needs of patients in this study and low needs for community and follow-up can be explained with meeting primary needs of the patients. In particular, adaptation of the patients having stroke for the first time to the new roles can take some time.
Considering the distribution of PLNS by age groups, the difference in sub-dimensions of community, follow-up and skin care among the age groups was found to be statistically significant (p < 0.05). Learning needs of the patients aged over 65 years from the community and follow-up and skin care sub-dimensions increased.
Learning needs of the aged patients were more than those of young ones in the study by A. Omari et al. [24]. In the literature, learning needs of the young patients were found to be high. Some studies, however, found no significant difference between the age variable and PLNS sub-dimensions [25].
Considering the relationship between genders, the scores were found to be similar in this study with 45.9 % for women and 54.1 % for men. Considering the PLNS distribution by gender, the difference was not statistically significant (p > 0.05).
The majority of the sampling group consisted of 40 (36.7 %) primary school graduate patients in the study. The group with the lowest number comprised illiterate patients with 10 people (9.2 %). In the training groups of this study, the difference between the PLNS sub-dimensions was not significant.
The importance of individual training should be underlined during discharge training. The sample of this study consisted of 70 married patients (64.2 %) and 39 single patients (35.8 %). Considering the PLNS distribution by mari–tal status, the difference was not statistically significant in the sub-dimensions (p > 0.05). Considering PLNS distribution in this study according to residential area, patients living with their spouse were 31 (28.4 %). The patients living with their spouse and children were 30 (27.5 %). The PLNS mean score was found to be high in the treatment and complications sub-dimension in the patients living with their spouse.
High scores of the patients living with their spouse from treatment and complications sub-dimensions can be explained with low education level of most patients and their being old, not knowing what to do in case of problems faced, not knowing the potential problems due to illness, not knowing how to do treatment follow-up and not foreseeing the potential side effects and complications post-treatment.
There are also such factors as presence of a chronic disease, use of drugs, smoking habits, the number of stroke, the length of hospital stay, whether the patients have received discharge training and who they have received discharge training from. The learning needs of non-smoking patients regarding medication, activities of living, community and follow-up, treatment and complications, and skin care have increased in the study. The learning needs of the patients who pointed that they received training from the nurse were high in all sub-dimensions. There was no significant difference between PLNS and the presence of chronic disease, use of medication, the number of strokes, length of hospital stay, and discharge training (p > 0.05).
Of the patients who comprised the sample group, 92 (84.4 %) had one or more chronic disease. The differences in the PLNS sub-dimensions were not found to be statistically significant (p > 0.05).
The stroke is a chronic disease and decreases self-management of individuals. What distinguishes stroke from other chronic diseases is that it comes unexpectedly and causes permanent sequel. This shows the necessity of learning needs of all patients with or without chronic disease after stroke.
Of the patients included in the study, 84 (77.1 %) are those using drugs. There was a statistically significant difference in the medication and PLNS sub-dimensions (p > 0.05).
The number of patients with smoking habits was 21 (19.3 %). The differences in the medication, activities of living, community and follow-up, treatment and complications, skin care. PLNS sub-dimensions and total scale scores were found to be statistically significant for the patients who did not smoke (p < 0.05). The PLNS sub-dimensions and total scale scores of the patients who did not smoke were higher than those who did.
Of the patients consisting the sample of the study, 77 (70.6 %) had only one stroke and 32 (29.4 %) had multiple strokes. The differences in the PLNS sub-dimensions according to the number of strokes were not found to be statistically significant (p > 0.05). Though not significant, the total scale scores of the patients having only one stroke from the PLNS were higher than those who had stroke more than once. This may have stemmed from the severity of stroke, obstacles caused and the anxiety that it might repeat. In the literature review, there was no study examining the relationship between stroke and PLNS.
Patient training is an important part of health care, and the studies have always underlined the dissatisfaction with patients in all aspects of health care, including the patients with stroke.
Distribution of PLNS Scores by the Length of Hospital Stay. The sample of the study mostly consisted of 54 (49.5 %) people, who were hospitalized for 5–14 days. This was followed by 52 patients (47.7 %) with duration of 1–5 days. There was no statistically significant difference in the length of hospital stay and PLNS sub-dimensions (p > 0.05).
PLNS Score Distribution According to Discharge Training. Of the patients, 49 (45 %) out of 109 patients stated that they received discharge training and 60 (55 %) did not receive. There was no statistically significant difference in the PLNS sub-dimensions according to have received discharge training (p > 0.05). Patients who have received discharge training need more training in the skin care sub-dimension compared to those who did not. Though not statistically significant, the PLNS total scale score of the patients who received discharge training was higher than the patients who did not. Thus, we can say that the patients’ training needs are not met enough.
Of the patients, 6 (5 %) out of 49 received discharge training from a doctor and 43 (39.1 %) from a nurse. Considering the patient learning needs according to the person who provided discharge training, all sub-dimension diffe–rences were found to be statistically significant (p < 0.05). In other words, both the PLNS total scale score and sub-dimension scores of the patients who received discharge training from nurses were higher than those who received from doctors.
Conclusions
In line with the results from the study, it is suggested to:
— Determine the subject to be provided to patients while planning patient education.
— Review the trainings on PLNS issues, considering the mean score obtained by the patients to be high.
— Design the trainings planned according to individual characteristics of the patients so as to increase the functionality of the trainings by paying attention to the discharge training.
— Organize more effective programs in discharge training, especially for undereducated patients.
— Provide discharge training to nurses through in-service trainings.
— Make discharge training, which is an indicator of a quality health service in institutions, a part of nursing practices.
— It is known that diabetes and its complications can be prevented or delayed with appropriate methods. For this reason, the implementation of effective policies developed at the national level, increasing the awareness of diabetes (actually all most common diseases that can cause stroke) in the society, preventing it at a high rate, providing adequate and appropriate education and treatment to the patients, reducing complications and paralysis and deaths due to diabetes, and with the successful implementation of the program, diabetes can be controlled in our country.
Received 04.05.2021
Revised 02.06.2021
Accepted 08.06.2021

/52.jpg)
/53.jpg)