Международный эндокринологический журнал Том 18, №2, 2022
Вернуться к номеру
Дефіцит магнію при цукровому діабеті 2-го типу та його вплив на глікемічний контроль та ускладнення цукрового діабету
Авторы: Savas Karatas, Yalcın Hacıoglu, Şennur Kose
Istanbul Research and Education Hospital, Fatih, Istanbul, Turkey
Рубрики: Эндокринология
Разделы: Клинические исследования
Версия для печати
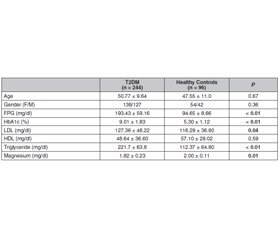
Актуальність. У світі спостерігається ріст захворюваності на цукровий діабет (ЦД). Магній належить до важливих елементів організму й виконує безліч життєво важливих функцій. Зараз відзначається тенденція досліджувати вплив магнію на патогенез ЦД 2-го типу та його ускладнення. У той же час потрібно більше доказів, щоб встановити взаємозв’язок між вмістом магнію та ЦД 2-го типу. Тому мета дослідження полягала у встановленні частоти дефіциту магнію в турецьких пацієнтів із ЦД 2-го типу та його впливу на глікемічний контроль та ускладнення ЦД. Матеріали та методи. У дослідження були залучені 296 пацієнтів із ЦД 2-го типу та 96 здорових осіб групи контролю віком 18–65 років. Після критеріїв виключення пацієнтів із ЦД 2-го типу розділили на дві групи за показником вмісту магнію, провели порівняння метаболічних характеристик пацієнтів обох груп. Також порівнювали частоту артеріальної гіпертензії, складових метаболічного синдрому, ішемічної хвороби серця та мікроальбумінурії залежно від наявності дефіциту магнію. Результати. Дефіцит магнію виявлений у 35,5 % (86/242) пацієнтів із ЦД 2-го типу, у 4,1 % (4/96) — у контрольній групі. Дефіцит магнію був більш вираженим у пацієнтів жіночої статі (64/86, 74,4 %). У чоловіків спостерігалася більша частота нормального рівня магнію — 89/166 (53,6 %) (p < 0,01). Пацієнти з ЦД 2-го типу зі зниженим вмістом магнію в крові вірогідно не відрізнялися за показником глікованого гемоглобіну HbA1c (9,0 ± 1,9 % проти 8,8 ± 1,6 %, p = 0,35) та рівнями глюкози в крові натще (197,24 ± 87,25 мг/дл проти 177,85 ± 57,22 мг/дл, p = 0,35). Пацієнти з ЦД 2-го типу зі зниженим вмістом магнію в крові мали вірогідно вищі рівні гіперліпідемії (48,8 % (42/86) проти 41,0 % (64/156), p = 0,04). Частота метаболічного синдрому (89,0 % (73/82) проти 83,1 % (123/148), p = 0,22) та ішемічної хвороби серця (39,5 % (34/86) проти 35,9 % (56/156), p = 0,85) не відрізнялася між групами обстежених. Частота артеріальної гіпертензії (81,4 % (70/86) проти 67,9 (60/156), p = 0,04) і мікроальбумінурії (66,7 % (38/57) проти 43,7 (58/119), p = 0,03) була вірогідно вищою в групі хворих на ЦД 2-го типу з низьким умістом магнію в крові. Висновки. Дефіцит магнію доволі часто спостерігається у хворих на ЦД 2-го типу, однак цей дефіцит вірогідно не впливає на глікемічний контроль. З іншого боку, встановлено, що частота артеріальної гіпертензії, мікроальбумінурії та гіперліпідемії зростає у хворих на ЦД 2-го типу з дефіцитом магнію.
Background. Diabetes has become more often in all over the world, magnesium is an essential element of the body and has lots of vital functions. There has been a trend to investigate magnesium’s effect on type 2 diabetes pathogenesis and its complications. Still, more data is needed to reveal magnesium and T2 diabetes mellitus (DM) association, therefore we aimed to investigate how common magnesium deficiency in Turkish T2DM patients, and its effect on diabetes control and diabetes complications. Materials and methods. 296 patients with type 2 DM and 96 healthy controls aged between 18–65 years were enrolled in the study. After exclusion criteria, T2DM patients were divided into 2 groups according to magnesium deficiency, metabolic and physical properties of the groups were compared. Also, hypertension, metabolic syndrome, coronary artery disease, and microalbuminuria were also compared according to magnesium deficiency. Results. Magnesium deficiency was found 35.5 % (86/242) in patients with type 2 DM, 4.1 % (4/96) in the control group. Magnesium deficiency was more in female patients (64/86, 74.4 %), male patients had more normal magnesium levels 89/166, 53.6 %) (p < 0.01). Hypomagnеsemia patients with T2 DM didn’t show difference in HbA1c (9.0 ± 1.9 % vs 8.8 ± 1.6 %, p = 0.35), and fasting blood glucose levels (197.24 ± 87.25 vs 177.85 ± 57.22 mg/dl, p = 0.14). Hypomagnеsemia patients with T2DM had significantly higher hyperlipidemia levels (48.8 % (42/86) vs 41.0 % (64/156), p = 0.04). Metabolic syndrome (89.0 % (73/82) vs 83.1 % (123/148), p = 0.22) and coronary artery syndrome (39.5 % (34/86) vs 35.9 % (56/156), p = 0.85) didn’t differ between groups. Hypertension (81.4 % (70/86) vs 67.9 (60/156), p = 0.04) and microalbuminuria (66.7 % (38/57) vs 43.7 (58/119), p = 0.03) were significantly higher in the hypomagnеsemia T2DM group. Conclusions. Magnesium deficiency is not rare in T2DM, however, this deficiency didn’t impact blood glucose control at a significant level in current study, on the other hand, hypertension, microalbuminuria, and hyperlipidemia components of diabetes have been shown to increase with magnesium deficiency.
цукровий діабет 2-го типу; магній; мікроальбумінурія
type 2 diabetes mellitus; magnesium; microalbuminuria
Introduction
Materials and methods
Results
Discussion
Conclusions
- de Baaij J.Н., Hoenderop J.G., Bindels R.J. Magnesium in man: implications for health and disease. Physiol. Rev. 2015 Jan. 95(1). 1-46. doi: 10.1152/physrev.00012.2014. PMID: 25540137.
- Zhang X., Xia J., Del Gobbo L.С., Hruby A., Dai Q., Song Y. Serum magnesium concentrations and all-cause, cardiovascular, and cancer mortality among U.S. adults: Results from the NHANES I Epidemiologic Follow-up Study. Clin. Nutr. 2018 Oct. 37(5). 1541-1549. doi: 10.1016/j.clnu.2017.08.021.
- Wesselink E. et al. Vitamin D, magnesium, calcium, and their interaction in relation to colorectal cancer recurrence and all-cause mortality. Am. J. Clin. Nutr. 2020 May 1. 111(5). 1007-1017. doi: 10.1093/ajcn/nqaa049.
- Larsson S.С. et al.; MEGASTROKE project of the International Stroke Genetics Consortium. Serum magnesium and calcium levels in relation to ischemic stroke: Mendelian randomization study. Neurology. 2019 Feb 26. 92(9). e944-e950. doi: 10.1212/WNL.0000000000007001.
- Shamnani G. et al. Correlation of Serum Magnesium with Insulin Resistance in North Indian Adult Population. Curr. Diabetes Rev. 2020. 16(3). 254-261. doi: 10.2174/1573399814666181016164432. PMID: 30332968.
- Luo X. et al. Associations of Serum Magnesium With Insulin Resistance and Testosterone in Women With Polycystic Ovary Syndrome. Front. Endocrinol. (Lausanne). 2021 Jun 23. 12. 683040. doi: 10.3389/fendo.2021.683040.
- Chutia H., Lynrah K.G. Association of Serum Magnesium Deficiency with Insulin Resistance in Type 2 Diabetes Mellitus. J. Lab. Physicians. 2015 Jul-Dec. 7(2). 75-8. doi: 10.4103/0974-2727.163131.
- Elderawi W.А., Naser I.А., Taleb M.Н., Abutair A.S. The Effects of Oral Magnesium Supplementation on Glycemic Response among Type 2 Diabetes Patients. Nutrients. 2018 Dec 26. 11(1). 44. doi: 10.3390/nu11010044.
- Dasgupta A., Sarma D., Saikia U.K. Hypomagnesemia in type 2 diabetes mellitus. Indian J. Endocrinol. Metab. 2012 Nov. 16(6). 1000-3. doi: 10.4103/2230-8210.103020.
- Azad K.M. et al. Serum magnesium in hospital admitted diabetic patients. Mymensingh Med. J. 2014 Jan. 23(1). 28-34. PMID: 24584369.
- Wälti M.К., Zimmermann M.В., Spinas G.А., Hurrell R.F. Low plasma magnesium in type 2 diabetes. Swiss Med. Wkly. 2003 May 17. 133(19–20). 289-92. PMID: 12844272.
- Lopez-Ridaura R. et al. Magnesium intake and risk of type 2 diabetes in men and women. Diabetes Care. 2004 Jan. 27(1). 134-40. doi: 10.2337/diacare.27.1.134. PMID: 14693979.
- Kao W.Н. et al. Serum and dietary magnesium and the risk for type 2 diabetes mellitus: the Atherosclerosis Risk in Communities Study. Arch. Intern. Med. 1999 Oct 11. 159(18). 2151-9. doi: 10.1001/archinte.159.18.2151. PMID: 10527292.
- Schutten J.C. et al. Lower Plasma Magnesium, Measured by Nuclear Magnetic Resonance Spectroscopy, is Associated with Increased Risk of Developing Type 2 Diabetes Mellitus in Women: Results from a Dutch Prospective Cohort Study. J. Clin. Med. 2019 Feb 1. 8(2). 169. doi: 10.3390/jcm8020169.
- Kostov K. Effects of Magnesium Deficiency on Mechanisms of Insulin Resistance in Type 2 Diabetes: Focusing on the Processes of Insulin Secretion and Signaling. Int. J. Mol. Sci. 2019 Mar 18. 20(6). 1351. doi: 10.3390/ijms20061351.
- Gommers L.М., Hoenderop J.G., Bindels R.J., de Baaij J.H. Hypomagnesemia in Type 2 Diabetes: A Vicious Circle? Diabetes. 2016 Jan. 65(1). 3-13. doi: 10.2337/db15-1028. PMID: 26696633.
- Manialawy Y., Khan S.R., Bhattacharjee A., Wheeler M.B. The magnesium transporter NIPAL1 is a pancreatic islet-expressed protein that conditionally impacts insulin secretion. J. Biol. Chem. 2020 Jul 17. 295(29). 9879-9892. doi: 10.1074/jbc.RA120.013277.
- Günther T. The biochemical function of Mg2+ in insulin secretion, insulin signal transduction and insulin resistance. Magnes. Res. 2010 Mar. 23(1). 5-18. doi: 10.1684/mrh.2009.0195.
- Zahra H. et al. Plasmatic Magnesium Deficiency in 101 Outpatients Living with Type 2 Diabetes Mellitus. Clin. Pract. 2021 Oct 27. 11(4). 791-800. doi: 10.3390/clinpract11040095.
- Odusan O.О. et al. Patterns and Correlates of Serum Magnesium Levels in Subsets of Type 2 Diabetes Mellitus Patients in Nigeria. Indian J. Endocrinol. Metab. 2017 May-Jun. 21(3). 439-442. doi: 10.4103/ijem.IJEM_190_16.
- Louvet L. et al. Characterisation of calcium phosphate crystals on calcified human aortic vascular smooth muscle cells and potential role of magnesium. PLoS One. 2015 Jan 21. 10(1). e0115342. doi: 10.1371/journal.pone.0115342.
- Villa-Bellosta R. Impact of magnesium:calcium ratio on calcification of the aortic wall. PLoS One. 2017 Jun 1. 12(6). e0178872. doi: 10.1371/journal.pone.0178872.
- Correa S. et al. Serum Magnesium, Blood Pressure, and Risk of Hypertension and Chronic Kidney Disease Progression in the CRIC Study. Hypertension. 2021 Dec. 78(6). 1771-1780. doi: 10.1161/HYPERTENSIONAHA.121.17694.
- Kaliaperumal R., Venkatachalam R., Nagarajan P., Sabapathy S.K. Association of Serum Magnesium with Oxidative Stress in the Pathogenesis of Diabetic Cataract. Biol. Trace Elem. Res. 2021 Aug. 199(8). 2869-2873. doi: 10.1007/s12011-020-02429-9.

/26.jpg)
/27.jpg)