Вступ
Якість життя (ЯЖ) — складне та широке поняття, що досі не має єдиного стійкого визначення через величезну вагу суб’єктивних чинників при його означенні [1]. Під ЯЖ, на думку дослідників, слід розуміти сукупність таких ознак: особистісний розвиток, міжособистісні стосунки, самовизначення, емоційне, фізичне та матеріальне благополуччя [1]. Якість життя, пов’язана зі здоров’ям (health-related quality of life — HRQOL), розглядає вплив основного захворювання та його лікування на життя пацієнта, включаючи фізичні, психічні та соціальні аспекти [2]. HRQOL виступає вагомою підставою для прийняття того чи іншого рішення щодо тактики лікування [2] і є вірогідно вищою при достатньому рівні фізичної активності [3]. У дітей із неврологічними проблемами тактика лікування, спрямована не лише на полегшення стану дитини, контроль клінічної симптоматики, а й на покращення якості її життя, має особливе значення [4, 5].
Частка дітей із неврологічними порушеннями в загальній популяції становить 6–9 % [6]. Батьки цієї категорії дітей більш схильні до психологічних проблем, їх часто переслідують відчуття невдачі, безпомічності та провини, у них високий рівень стресу, розлади соматичного здоров’я. Стосунки в родині після народження дітей із порушеннями психомоторного розвитку здебільшого різко погіршуються [1, 6–8]. ЯЖ здорових братів та сестер дітей із неврологічною патологією часто також суттєво страждає [9]. Значення для ЯЖ мають також місце проживання родини та етнічна приналежність [10]. Великою проблемою для таких сімей у цей час стає брак або відсутність підтримки з боку соціальних служб, втрата роботи [1, 11, 12].
За даними досліджень, показники якості життя батьків неврологічно здорових дітей були вірогідно вищими, ніж у батьків дітей із порушеннями психомоторного розвитку. Також показники ЯЖ сімей дітей із неврологічними проблемами мали залежність від статі (у батьків були вірогідно вищими, ніж у матерів) та рівня освіти (вищий рівень освіти асоціювався з вірогідно вищими показниками ЯЖ), працевлаштування та сімейного доходу [1, 11], а також від стратегії подолання труднощів, застосованої в них [11, 13–15]. Терапевтичні втручання із залученням доглядальників мають виражений сприятливий вплив на їхню ЯЖ [16–18].
Здатність родини адаптуватися в цих умовах є невід’ємною передумовою забезпечення інтеграції дитини з неврологічними порушеннями в суспільство, її емоційного та виконавчого функціонування [6, 19].
Серед соматичних проблем зі здоров’ям у дітей із неврологічною патологією найчастіше виявлялися: надмірна маса тіла та ожиріння, проблеми із зором, порушення нутритивного статусу, нетримання сечі та калу [20], які сприяють зниженню якості життя дітей та їхніх батьків, ускладнюють перебіг основного захворювання та реабілітаційні заходи [21].
Розлади аутистичного спектра (РАС) — група неврологічних розладів із труднощами в соціальних взаєминах, порушенням комунікативних навичок, повторюваною та стереотипною поведінкою, а також значним впливом на життя дитини та її родини. Нозологія проявляється високим рівнем стресу батьків та незадоволеності соціальними та медичними послугами, які надаються їхнім дітям, поєднується із порушеннями соціально-економічного статусу, підвищеним ризиком втрати ними роботи [22–28].
Рівень стресу в батьків дітей із РАС обернено пропорційний віку дітей [29]. У сім’ях частим явищем є порушення емоційного контакту з дитиною, дистанціювання від неї [30]. Не менш поширеними є відчуття горя, тривожності та депресії. Матері цієї категорії дітей були більш схильними до тривожних та депресивних розладів, частіше відзначали зниження психологічного комфорту; разом із тим у батьків спостерігалося підвищення артеріального тиску та варіабельності серцевого ритму [31–33].
Dawn Adams et al. у своїй роботі доводять наявність зворотної залежності між вираженістю тривожної симптоматики в дітей із РАС та ЯЖ дітей та їхніх родин [34].
У матерів-одиначок виникали додаткові труднощі з пошуком роботи із гнучким графіком [35]. В іншому дослідженні вірогідної різниці між рівнем стресу в батьків та матерів не було виявлено [36]. Якість життя матерів дітей із РАС, на відміну від батьків, вірогідно частіше погіршувалася через наявні в дітей із РАС порушення соціальних функцій [28]. Для родин дітей із неврологічною патологією, зокрема з РАС, найтяжчим вважається перший рік від моменту встановлення дітям діагнозу [37]. Ознаки посттравматичного стресового розладу спостерігаються у 20 % батьків після встановлення в їхніх дітей діагнозу РАС [38]. Причиною цього є труднощі, що виникають у стосунках між дітьми та їх батьками. Величезним викликом для батьків є потреба постійного поєднання піклування про дитину та щоденної діяльності [39].
Для батьків дітей із РАС першочергове значення має здатність їхніх дітей до самообслуговування, незалежність у побуті, сприйняття з боку суспільства, можливість бути почутими та знайти розуміння в медпрацівників і співробітників соціальних служб. Наявність цих передумов сприяє зменшенню розчарування та відчаю, які домінують серед емоцій у батьків дітей із РАС [31, 40–42]. Негативний вплив на якість життя дітей із РАС та їхніх батьків мають соматичні та стоматологічні проблеми, супутні психіатричні розлади [43–46], знижені навички самообслуговування [47–49]. Виявлено негативний вплив на ЯЖ дітей із РАС порушень великої моторики [50], втрати функцій та поведінкових проблем [51] та сприятливий вплив терапевтичних втручань, пов’язаних із фізичною активністю [52].
Синдром дефіциту уваги з гіперактивністю (СДУГ) належить до порушень психомоторного розвитку дитячого віку, частота якого значно зросла останніми роками. СДУГ є одним із важливих чинників, здатних вплинути на успіхи дитини в житті та навчанні, її моральне та фізичне благополуччя, здатність зав’язувати соціальні контакти [53, 54]. Характеризується проявами неуважності, надмірної активності та імпульсивності, які не відповідають рівню розвитку дитини [55]. Діти зі СДУГ та їхні родини мали вірогідно нижчі значення показників якості життя порівняно із здоровими однолітками та їх родинами [56]. Вплив СДУГ на ЯЖ дітей часто є порівнянним із впливом на неї бронхіальної астми чи цукрового діабету у відповідної категорії пацієнтів [57]. Найбільше страждали психосоціальні аспекти якості життя дітей зі СДУГ, негативний вплив на фізичні аспекти був значно менший [58].
Прямий вплив на показники ЯЖ цієї категорії пацієнтів мають розлади сну [59, 60] та порушення виконавчого функціонування [61]. В іншому дослідженні в батьків дітей зі СДУГ спостерігалися середні показники якості життя, а більшість опитаних сімей були неблагополучними [62]. У таких сім’ях переважала замкнута поведінка в обох батьків, що призводило до стрімкого погіршення психологічного клімату в родині, високого рівня стресу [23, 63, 64].
Депресивні розлади в осіб, що доглядають цю групу дітей, корелюють із погіршенням у них клініки основного захворювання [65]. У батьків дітей зі СДУГ спостерігалися вірогідно вищі рівні стресу, тривожності та депресивних розладів, ніж у групі батьків дітей із РАС [66]. Дослідження підтверджують наявність вірогідно вищого рівня стигматизації осіб жіночої статі, які доглядали дівчаток зі СДУГ, порівняно з особами чоловічої статі, які доглядали хлопчиків зі СДУГ. Вищий рівень стигматизації частіше зустрічався в дітей із вираженою клінікою СДУГ, негативним ставленням з боку їх доглядальників до самого захворювання та його лікування, а також з вищим освітнім рівнем цих осіб [67]. Інші дослідження також підтверджують наявність більшого навантаження, що лягає на плечі матерів дітей зі СДУГ [68, 69]. Велике значення має корекція депресивної симптоматики [70].
Серед дитячої популяції зростає частка дітей із затримкою психомовленнєвого розвитку (ЗПМР) [71]. Родини дітей із ЗПМР стикаються з тими ж проблемами, що й родини дітей із РАС та СДУГ, зокрема, при наявності значного інтелектуального дефіциту [72, 73]. Домінуюча позиція тут належить стресовим явищам у стосунках між батьками й дітьми, обумовленим розчаруванням та труднощами в комунікації між ними, які опосередковують підвищення частоти несприятливих поведінкових реакцій у дітей із затримкою психомовленнєвого розвитку [74]. Ця категорія дітей вразлива до впливу негативних наслідків на стан здоров’я та несприятливих соціально-економічних чинників [75, 76].
В основі розвитку мінімальної мозкової дисфункції (ММД) лежать як генетична схильність, так і органічне ураження ЦНС в ранньому віці. Вона включає поведінкові розлади, розгальмованість, підвищену збудливість, проблеми із самоконтролем, некерованість та агресивність, що негативно впливають на ЯЖ дітей з цією нозологією та їх батьків [77].
Значною проблемою залишається доступність медичних послуг для дітей із порушеннями психомоторного розвитку та їх родин. Підвищення їхньої якості сприятиме економії ресурсів, більшій продуктивності, інклюзивності та економічній доцільності [78, 79].
Для багатьох країн, що розвиваються, є характерними зменшення кількості медичних закладів та поганий стан транспортної інфраструктури, що створює додаткові бар’єри при зверненні за медичною допомогою батьків дітей із неврологічною патологією [80]. Схожу ситуацію можемо спостерігати і в нашій країні, зокрема поза межами великих міст та у віддаленій сільській місцевості [81]. Важливими факторами є відстань до лікувальної установи, якість надання медичних послуг, захист особистих даних, навички міжособистісного спілкування медпрацівників [73, 82].
Висока частота коморбідних нозологій у дітей із порушеннями психомоторного розвитку спричиняє вірогідно вищу частоту звернень до медичних установ та госпіталізацій до стаціонару [83, 84]. Ситуацію ускладнює висока вартість терапевтичних та корекційних заходів, економічний тягар яких відчутний навіть для економік розвинутих країн і в майбутньому лише збільшуватиметься [85, 86]. Якнайшвидша діагностика у дитини порушень психомоторного розвитку, впровадження ефективних терапевтичних стратегій консультування родин, адекватна соціальна підтримка з боку держави дозволять покращити якість життя цієї категорії дітей та їхніх батьків [87].
Мета дослідження: оцінити якість життя дітей із порушеннями психомоторного розвитку та їхніх родин, вплив на родину наявних у дітей психомоторних порушень, а також доступність медичної допомоги та задоволення якістю її надання цій категорії пацієнтів; виявити зв’язок між обрахованими показниками якості життя дітей та їх родин і наявними у них порушеннями психомоторного розвитку.
Матеріали та методи
Проаналізовані результати анкетування батьків 45 дітей дошкільного віку (3–7 років) — пацієнтів неврологічного відділення КНП «Міська дитяча клінічна лікарня м. Львова» та вихованців навчально-розвивального Монтессорі-центру «Сонячний промінчик». Анкетування батьків проводили за допомогою опитувальників PedsQLTM 2.0 Family Impact Module (включає такі блоки запитань: «Фізичне функціонування», «Емоційне функціонування», «Соціальне функціонування», «Розумове функціонування», «Спілкування», «Занепокоєння», «Повсякденна діяльність», «Відносини у родині», «Підсумковий бал якості життя батьків, пов’язаний із станом здоров’я» (The Parent HRQL Summary Score — включає суму балів із блоків «Фізичне функціонування», «Емоційне функціонування», «Соціальне функціонування» та «Розумове функціонування», поділену на кількість відповідей на запитання в цих блоках), «Підсумковий бал функціонування родини» (The Family Functioning Summary Score — включає суму балів із блоків «Повсякденна діяльність» та «Відносини у родині»), а також «Загальний бал»), PedsQLTM 4.0 Generic Score Scales (Parent Report for Toddlers (ages 2–4) та Parent Report for Young Children (ages 5–7)), що складаються з таких блоків запитань: «Фізичне функціонування», «Емоційне функціонування», «Соціальне функціонування», «Функціонування у школі/дитячому садку», «Підсумковий бал психосоціального здоров’я» (Psychosocial Health Summary Score — є сумою балів у рубриках «Емоційне функціонування», «Соціальне функціонування» та «Функціонування в школі/дитячому садку», розділеною на кількість відповідей на запитання у цих рубриках), «Підсумковий бал фізичного здоров’я» (Physical Health Summary Score —дорівнює «Фізичному функціонуванню»), «Загальний бал», PedsQLTM Healthcare Satisfaction Generic Module (містить рубрики «Обізнаність», «Залучення сім’ї», «Комунікація», «Технічні навички», «Емоційні потреби», «Загальне задоволення», «Загальний бал»), наданих безкоштовно на підставі користувацької угоди французькою неприбутковою організацією Mapi Research Trust (автор та укладач опитувальників — доктор Джеймс Варні (Dr. James W. Varni)) та перекладених українською мовою. Після конвертації пунктів в опитувальниках за 100-бальною шкалою відбувалося визначення середніх значень за кожним блоком опитувальників. Статистична обробка включала розрахунки із використанням кореляційного та параметричного аналізу. Кореляційний аналіз включав визначення коефіцієнта рангової кореляції Спірмена з визначенням сили й напрямку кореляції для виявлення зв’язку між середніми значеннями показників якості життя дітей за бальною шкалою та наявними у них порушеннями психомоторного розвитку. Вірогідність коефіцієнта рангової кореляції оцінювалася за допомогою розрахунку середньої похибки рангового коефіцієнта кореляції та визначенням критерію вірогідності (t-критерій Стьюдента). Для обрахунків проведено рангування ряду отриманих середніх значень в порядку зростання. Обстежені діти були ранговані за наявною в них неврологічною патологією, згодом визначалися відхилення значень рядів та сума їх відхилень, піднесених до квадрата. Отримані значення застосовувалися для визначення рангового коефіцієнта кореляції, його середньої похибки та критерію вірогідності (t-критерію Стьюдента) з врахуванням числа ступенів свободи варіаційних рядів для порівнюваних груп дітей у кожному блоці запитань, а також статі дітей. Також визначалася вірогідність різниці між середніми значеннями конвертованих за 100-бальною шкалою показників кожного блоку запитань в опитувальниках з урахуванням статі дітей шляхом критерію вірогідності (t-критерію Стьюдента) з врахуванням числа ступенів свободи варіаційних рядів для порівнюваних груп дітей. Середні величини подані у вигляді (M ± m), де М — середнє значення показника, m — стандартна похибка середнього; n — обсяг аналізованої групи. Для статистичної обробки використана комп’ютерна програма «Біостат». Відмінності між групами пацієнтів вважалися вірогідними при р < 0,05. Дослідження було виконано відповідно до принципів Гельсінської декларації. Протокол дослідження було затверджено Комісією з питань етики наукових досліджень, експериментальних розробок і наукових творів ЛНМУ імені Данила Галицького. На проведення дослідження було отримано інформовану згоду батьків дітей (або їхніх опікунів).
Результати
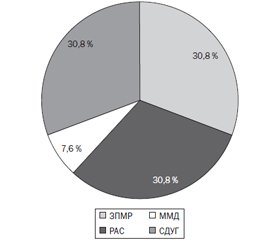
Анкетування батьків проводили за допомогою опитувальників PedsQLTM 2.0 Family Impact Module, PedsQLTM 4.0 Generic Score Scales (Parent Report for Toddlers (ages 2–4) та Parent Report for Young Children (ages 5–7)) та PedsQLTM Healthcare Satisfaction Generic Module. До обстежуваної групи входили 45 дітей дошкільного віку (3–7 років, середній вік — 4,2 ± 0,2 року) — пацієнтів неврологічного відділення КНП «Міська дитяча клінічна лікарня м. Львова» та вихованців навчально-розвивального Монтессорі-центру «Сонячний промінчик» (із них 32 хлопчики (71,1 %), середній вік — 3,9 ± 0,2 року, та 13 дівчаток (28,9 %), середній вік — 4,8 ± 0,3 року (рис. 1)) із порушеннями психомоторного розвитку (затримкою психомовленнєвого розвитку — 21 хлопчик (65,6 %) та 4 дівчинки (30,8 %) (рис. 2, 3); розладами аутистичного спектра — 5 хлопчиків (15,6 %) і 4 дівчинки (30,8 %) (рис. 2, 3); мінімальною мозковою дисфункцією — 3 хлопчики (9,4 %) та 1 дівчинка (7,6 %) (рис. 2, 3); синдромом дефіциту уваги з гіперактивністю — 3 хлопчики (9,4 %) і 4 дівчинки (30,8 %) (рис. 2, 3)). Щоденний догляд за практично всіма обстеженими дітьми із психомоторними порушеннями (за винятком однієї дитини) здійснювався переважно зусиллями їхніх матерів. Родини всіх обстежених дітей були повними, у всіх родинах обидва батьки мали вищу освіту.
/9.jpg)
При визначенні кореляційного зв’язку між даними анкетування батьків і неврологічними порушеннями в дітей встановлено: наявність сильного прямого вірогідного зв’язку між середніми показниками батьків хлопчиків із ЗПМР та наявною в їхніх дітей неврологічною патологією у рубриці «Емоційне функціонування» опитувальника PedsQLTM 2.0 Family impact module (р < 0,01); у батьків хлопчиків із РАС у цій же рубриці даного опитувальника виявлено слабку пряму невірогідну кореляцію (p > 0,05); у батьків хлопчиків із ММД у цій же рубриці даного опитувальника — середньої сили зворотну невірогідну кореляцію (p > 0,05); у батьків хлопчиків зі СДУГ цієї ж рубрики даного опитувальника — кореляція відсутня; між бальними оцінками батьків усіх обстежених хлопчиків у рубриці «Емоційне функціонування» даного опитувальника та неврологічними проблемами у їхніх дітей — сильну пряму вірогідну кореляцію (р < 0,01); у батьків дівчаток із ЗПМР та СДУГ у рубриці «Емоційне функціонування» даного опитувальника — середньої сили зворотну невірогідну кореляцію (p > 0,05); у батьків дівчаток із РАС у цій же рубриці — середньої сили пряму невірогідну кореляцію (p > 0,05); серед обстежених дітей лише в однієї дівчинки було діагностовано ММД; між бальними оцінками батьків усіх обстежених дівчаток у рубриці «Емоційне функціонування» даного опитувальника та психомоторними розладами у дітей — пряму середньої сили невірогідну кореляцію (p > 0,05).
/10.jpg)
У рубриці «Фізичне функціонування» у батьків хлопчиків із ЗПМР та РАС верифіковано слабку пряму невірогідну кореляцію з присутньою в дітей неврологічною патологією (p > 0,05); у батьків хлопчиків із ММД — зворотну слабку невірогідну кореляцію (p > 0,05); у батьків хлопчиків зі СДУГ кореляція була відсутньою; між бальними оцінками батьків всіх обстежених хлопчиків у цій рубриці та неврологічними проблемами у дітей — середньої сили пряма вірогідна кореляція (р < 0,01); у батьків дівчаток із ЗПМР у цій рубриці — слабка зворотна невірогідна кореляція (p > 0,05); у батьків дівчаток із РАС — середньої сили пряма невірогідна кореляція (p > 0,05); у батьків дівчаток із СДУГ — середньої сили зворотна невірогідна кореляція (p > 0,05); у батьків всіх обстежених дівчаток у цій рубриці та наявною в дітей неврологічною патологією встановлена середньої сили пряма невірогідна кореляція (p > 0,05).
У рубриці «Соціальне функціонування» у батьків хлопчиків із ЗПМР кореляційний зв’язок з неврологічними проблемами їхніх дітей був слабким прямим невірогідним (p > 0,05); аналогічна ситуація спостерігалася і у хлопчиків із РАС (p > 0,05); у хлопчиків із ММД — зв’язок слабкий зворотний невірогідний (p > 0,05); у хлопчиків зі СДУГ — відсутній; у всіх обстежених хлопчиків у цій рубриці — середньої сили прямий невірогідний зв’язок (p > 0,05); у дівчаток із ЗПМР та РАС у даній рубриці — середньої сили прямий невірогідний (p > 0,05); у дівчаток зі СДУГ — сильний зворотний невірогідний (p > 0,05); у всіх обстежених дівчаток в цій рубриці — середньої сили прямий вірогідний (р < 0,05).
У батьків хлопчиків із ЗПМР та РАС у рубриці «Розумове функціонування» виявлялася середньої сили пряма невірогідна кореляція з психомоторними порушеннями в дітей (p > 0,05); у батьків хлопчиків із ММД — середня зворотна невірогідна (p > 0,05); у батьків хлопчиків зі СДУГ — відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — середньої сили пряма вірогідна кореляція (р < 0,05). У батьків дівчаток із ЗПМР у даній рубриці — сильна пряма невірогідна кореляція (р > 0,05); у батьків дівчаток із РАС та у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряма невірогідна кореляція з неврологічною патологією у їхніх дітей (р > 0,05); у батьків дівчаток зі СДУГ — середньої сили зворотна невірогідна кореляція (р > 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Спілкування» спостерігалася слабка пряма невірогідна кореляція з наявною в дітей неврологічною патологією (р > 0,05); у батьків хлопчиків із РАС та ММД — пряма середньої сили невірогідна кореляція (р > 0,05); у батьків хлопчиків зі СДУГ — кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — середньої сили пряма вірогідна кореляція (р < 0,01). У батьків дівчаток із ЗПМР та СДУГ у даній рубриці — середньої сили зворотна невірогідна кореляція (р > 0,05); у батьків дівчаток з РАС — слабка пряма невірогідна кореляція (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01).
У батьків хлопчиків із ЗПМР у рубриці «Занепокоєння» верифіковано середньої сили пряму вірогідну кореляцію з психомоторними порушеннями у дітей (р < 0,05); у батьків хлопчиків з РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01). У батьків дівчаток із ЗПМР та СДУГ у цій же рубриці — середньої сили зворотна невірогідна кореляція (р > 0,05); у батьків дівчаток із РАС — середньої сили пряма невірогідна кореляція (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряма невірогідна кореляція (р > 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Повсякденна діяльність» виявлено середньої сили пряму невірогідну кореляцію з неврологічною патологією у дітей (р > 0,05); у батьків хлопчиків із РАС — сильну пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у всіх обстежених хлопчиків у цій рубриці виявлено сильну пряму вірогідну кореляцію (р < 0,01). У батьків дівчаток із ЗПМР та СДУГ у цій же рубриці — середньої сили зворотну невірогідну кореляцію (р > 0,05); у батьків дівчаток із РАС — слабку пряму невірогідну кореляцію (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — сильну пряму вірогідну кореляцію (р < 0,01).
У батьків хлопчиків із ЗПМР та РАС у рубриці «Відносини в родині» верифіковано слабку пряму невірогідну кореляцію з неврологічними порушеннями (р > 0,05); у батьків хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці виявлено середню пряму вірогідну кореляцію (р < 0,01). У батьків дівчаток із ЗПМР та СДУГ у цій же рубриці встановлено середньої сили зворотну невірогідну кореляцію (р > 0,05); у батьків дівчаток з РАС — сильну пряму невірогідну кореляцію (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — слабку зворотну невірогідну кореляцію (р > 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Підсумковий бал якості життя батьків, пов’язаний із станом здоров’я» (The Parent HRQL Summary Score) виявлено сильну зворотну вірогідну кореляцію з психомоторними порушеннями (р < 0,01); у батьків хлопчиків із РАС — слабку пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків із ММД — сильну пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці встановлено середньої сили зворотну вірогідну кореляцію (р < 0,01). У батьків дівчаток із ЗПМР та СДУГ у цій же рубриці — середньої сили зворотну невірогідну кореляцію (р > 0,05); у батьків дівчаток із РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середньої сили зворотну невірогідну (р > 0,05).
У батьків хлопчиків із ЗПМР та ММД у рубриці «Підсумковий бал функціонування родини» (The Family Functioning Summary Score) спостерігається слабка зворотна невірогідна кореляція з неврологічними порушеннями (р > 0,05); у батьків хлопчиків із РАС — слабка пряма невірогідна кореляція (р > 0,05); у батьків дітей зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — слабка пряма невірогідна кореляція (р > 0,05). У батьків дівчаток із ЗПМР та РАС у цій же рубриці — середньої сили пряма невірогідна кореляція (р > 0,05); у батьків дівчаток зі СДУГ — середньої сили зворотна невірогідна кореляція (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — слабка зворотна невірогідна кореляція (р > 0,05).
У батьків хлопчиків із ЗПМР і ММД у рубриці «Загальний бал» (Total score) верифіковано зворотну слабку невірогідну кореляцію з неврологічною патологією (р > 0,05); у батьків хлопчиків з РАС — сильну пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція була відсутня; у батьків всіх обстежених хлопчиків у цій рубриці встановлено слабку пряму невірогідну кореляцію (р > 0,05). У батьків дівчаток із ЗПМР і СДУГ у цій же рубриці Total score — середньої сили зворотну невірогідну кореляцію (р > 0,05); у батьків дівчаток із РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середню зворотну невірогідну кореляцію (р > 0,05).
У батьків хлопчиків із ЗПМР і РАС у рубриці «Обізнаність» опитувальника PedsQLTM Healthcare Satisfaction Generic Module виявлено середню пряму вірогідну кореляцію із психомоторними порушеннями в дітей (р < 0,05); у батьків хлопчиків з ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція була відсутня; у батьків всіх обстежених хлопчиків у цій же рубриці — середньої сили пряму вірогідну кореляцію (р < 0,01). У батьків дівчаток із ЗПМР і СДУГ у рубриці «Обізнаність» — середньої сили зворотну невірогідну кореляцію (р > 0,05); у батьків дівчаток із РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряму вірогідну кореляцію (р < 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Залучення сім’ї» спостерігається середньої сили пряма невірогідна кореляція з наявною неврологічною патологією (р > 0,05); в батьків хлопчиків із РАС — слабка пряма невірогідна кореляція (р > 0,05); у батьків хлопчиків з ММД — слабка зворотна невірогідна кореляція (р > 0,05); у батьків хлопчиків зі СДУГ кореляція була відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01). У батьків дівчаток із ЗПМР в рубриці «Залучення сім’ї» — середньої сили зворотна невірогідна кореляція (р > 0,05); у батьків дівчаток із РАС — сильна пряма невірогідна кореляція (р > 0,05); у батьків дівчаток зі СДУГ — сильна зворотна невірогідна кореляція (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряма невірогідна кореляція (р > 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Комунікація» виявлено середньої сили пряму невірогідну кореляцію з неврологічними проблемами (р > 0,05); у батьків хлопчиків із РАС — сильну пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — середньої сили пряма вірогідна кореляція (р < 0,01). У батьків дівчаток із ЗПМР в рубриці «Комунікація» — слабка пряма невірогідна кореляція (р > 0,05); у батьків дівчаток із РАС — середня пряма невірогідна кореляція (р > 0,05); у батьків дівчаток зі СДУГ — середня зворотна невірогідна кореляція (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряма вірогідна кореляція (р < 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Технічні навички» верифіковано середньої сили пряму вірогідну кореляцію з психомоторними порушеннями (р < 0,01); у батьків хлопчиків із РАС — сильну пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01). У батьків дівчаток із ЗПМР у рубриці «Технічні навички» — середньої сили зворотна невірогідна кореляція (р > 0,05); у батьків дівчаток із РАС — сильна пряма невірогідна кореляція (р > 0,05); у батьків дівчаток зі СДУГ кореляція була відсутня; у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряма вірогідна кореляція (р < 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Емоційні потреби» спостерігається сильна пряма вірогідна кореляція з наявними неврологічними порушеннями (р < 0,01); у батьків хлопчиків із РАС — сильна пряма невірогідна кореляція (р > 0,05); у батьків хлопчиків із ММД — слабка зворотна невірогідна кореляція (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01). У батьків дівчаток із ЗПМР та СДУГ цієї ж рубрики — середня зворотна невірогідна кореляція (р > 0,05); у батьків дівчаток із РАС — середньої сили пряма невірогідна кореляція (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряма вірогідна кореляція (р < 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Загальне задоволення» виявлено сильну пряму вірогідну кореляцію з неврологічними проблемами (р < 0,01); у батьків хлопчиків із РАС — сильну пряму невірогідну кореляцію (р > 0,05); у батьків хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у батьків хлопчиків зі СДУГ кореляція відсутня; у батьків всіх обстежених хлопчиків у цій рубриці встановлено сильну пряму вірогідну кореляцію (р < 0,01). У батьків дівчаток із ЗПМР та СДУГ у цій рубриці — середньої сили зворотну невірогідну кореляцію (р > 0,05); у батьків дівчаток з РАС — сильну пряму невірогідну кореляцію (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — середньої сили пряму вірогідну кореляцію (р < 0,05).
У батьків хлопчиків із ЗПМР у рубриці «Загальний бал» (Total score) спостерігається сильна зворотна вірогідна кореляція з психомоторними порушеннями (р < 0,01); у батьків хлопчиків із РАС — середня зворотна невірогідна кореляція (р > 0,05); у батьків хлопчиків із ММД — слабка зворотна невірогідна кореляція (р > 0,05); у батьків хлопчиків зі СДУГ кореляція була відсутньою; у батьків всіх обстежених хлопчиків у цій рубриці — середньої сили зворотна вірогідна кореляція (р < 0,01). В батьків дівчаток із ЗПМР та СДУГ у рубриці «Загальний бал» (Total score) — середньої сили зворотна невірогідна кореляція (р > 0,05); у батьків дівчаток із РАС — середньої сили пряма невірогідна кореляція (р > 0,05); у батьків всіх обстежених дівчаток у цій рубриці — слабка пряма невірогідна кореляція (р > 0,05).
У хлопчиків із ЗПМР у рубриці «Фізичне функціонування» опитувальника PedsQLTM 4.0 Generic Score Scales, а також у всіх обстежених хлопчиків у цій рубриці верифіковано середньої сили пряму вірогідну кореляцію (р < 0,01); в хлопчиків із РАС — слабку пряму невірогідну кореляцію (р > 0,05); у хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у хлопчиків зі СДУГ кореляції не виявлено. У дівчаток із ЗПМР та РАС у цій же рубриці, а також у всіх обстежених дівчаток у цій рубриці встановлено середню пряму невірогідну кореляцію (р > 0,05); у дівчаток зі СДУГ — середньої сили зворотну невірогідну кореляцію (р > 0,05).
У хлопчиків із ЗПМР у рубриці «Емоційне функціонування» виявлено середню пряму вірогідну кореляцію (р < 0,05); у хлопчиків із РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у хлопчиків із ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у хлопчиків зі СДУГ кореляції не виявлено; у всіх обстежених хлопчиків у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01). У дівчаток із ЗПМР і СДУГ у рубриці «Емоційне функціонування» — середня зворотна невірогідна кореляція (р > 0,05); у дівчаток із РАС — сильна пряма невірогідна кореляція (р > 0,05); у всіх обстежених дівчаток у цій рубриці — середньої сили пряма невірогідна кореляція (р > 0,05).
У хлопчиків із ЗПМР у рубриці «Соціальне функціонування» спостерігається середньої сили пряма вірогідна кореляція (р < 0,05); у хлопчиків з РАС — слабка пряма невірогідна кореляція (р > 0,05); у хлопчиків із ММД — слабка зворотна невірогідна кореляція (р > 0,05); у хлопчиків зі СДУГ кореляції не виявлено; у всіх обстежених хлопчиків у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01). В дівчаток із ЗПМР та СДУГ в рубриці «Соціальне функціонування» — середня зворотна невірогідна кореляція (р > 0,05); у дівчаток із РАС — середня пряма невірогідна кореляція (р > 0,05); в усіх обстежених дівчаток у цій рубриці — слабка пряма невірогідна кореляція (р > 0,05).
У хлопчиків із ЗПМР в рубриці «Функціонування у школі/дитячому садку» верифікується сильна пряма вірогідна кореляція (р < 0,01); у хлопчиків з РАС — слабка пряма невірогідна кореляція (р > 0,05); у хлопчиків із ММД — слабка зворотна невірогідна кореляція (р > 0,05); у хлопчиків зі СДУГ кореляція була відсутньою; в усіх обстежених хлопчиків у цій рубриці — сильна пряма вірогідна кореляція (р < 0,01). У дівчаток із ЗПМР у рубриці «Функціонування у школі/дитячому садку» — слабка пряма невірогідна кореляція (р > 0,05); у дівчаток із РАС — сильна пряма невірогідна кореляція (р > 0,05); у дівчаток зі СДУГ — слабка зворотна невірогідна кореляція (р > 0,05); в усіх обстежених дівчаток у даній рубриці — сильна пряма вірогідна кореляція (р < 0,01).
У хлопчиків із ЗПМР у рубриці «Підсумковий бал психосоціального здоров’я» (Psychosocial Health Summary) виявлено середньої сили зворотну вірогідну кореляцію (р < 0,01); в хлопчиків із РАС — слабку пряму невірогідну кореляцію (р > 0,05); в хлопчиків з ММД — слабку зворотну невірогідну кореляцію (р > 0,05); в хлопчиків зі СДУГ кореляції не виявлено; в усіх обстежених хлопчиків в даній рубриці встановлено середню зворотну вірогідну кореляцію (р < 0,01). У дівчаток із ЗПМР та СДУГ в рубриці «Підсумковий бал психосоціального здоров’я» (Psychosocial Health Summary) — середньої сили зворотну невірогідну кореляцію (р > 0,05); в дівчаток із РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у всіх обстежених дівчаток в цій рубриці — середньої сили зворотну невірогідну кореляцію (р > 0,05).
У хлопчиків із ЗПМР у рубриці «Підсумковий бал фізичного здоров’я» (Physical Health Summary Score) спостерігається середня пряма вірогідна кореляція (р < 0,05); у хлопчиків з РАС — слабка пряма невірогідна кореляція (р > 0,05); у хлопчиків з ММД — зворотна слабка невірогідна кореляція (р > 0,05); у хлопчиків зі СДУГ кореляція була відсутньою; у всіх обстежених хлопчиків у цій рубриці встановлено середньої сили пряму вірогідну кореляцію (р < 0,01). У дівчаток із ЗПМР та СДУГ у рубриці «Підсумковий бал фізичного здоров’я» (Physical Health Summary Score) виявлено середньої сили зворотну невірогідну кореляцію (р > 0,05); в дівчаток з РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у всіх обстежених дівчаток в цій рубриці — середньої сили пряму невірогідну кореляцію (р > 0,05).
У хлопчиків із ЗПМР у рубриці «Загальний бал» (Total score) верифіковано сильну зворотну вірогідну кореляцію (р < 0,01); у хлопчиків із РАС та ММД — слабку зворотну невірогідну кореляцію (р > 0,05); у хлопчиків зі СДУГ кореляція була відсутньою; у всіх обстежених хлопчиків в цій рубриці встановлено середньої сили зворотну вірогідну кореляцію (р < 0,01). В дівчаток із ЗПМР та СДУГ у цій же рубриці — середньої сили зворотну невірогідну кореляцію (р > 0,05); у дівчаток із РАС — середньої сили пряму невірогідну кореляцію (р > 0,05); у всіх обстежених дівчаток у цій рубриці — середньої сили зворотну невірогідну кореляцію (р > 0,05).
За даними опитувальника PedsQLTM 2.0 Family impact module, у рубриці «Підсумковий бал якості життя батьків, пов’язаний із станом здоров’я» (The Parent HRQL Summary Score) спостерігалася вірогідна різниця між показниками в родинах хлопчиків та дівчаток (у сім’ях хлопчиків середні значення були вірогідно вищими, ніж у дівчаток) (р < 0,01).
За даними опитувальника PedsQLTM Healthcare Satisfaction Generic Module, у рубриці «Обізнаність» середні значення у родинах хлопчиків були вірогідно вищими, ніж у родинах дівчаток (р < 0,01). В рубриці «Загальний бал» (Total score) цього ж опитувальника середні значення у сімей хлопчиків були вірогідно вищими, ніж у сімей дівчаток (р < 0,01).
Між показниками родин хлопчиків із ЗПМР та ММД у рубриці «Емоційне функціонування» опитувальника PedsQLTM 2.0 Family impact module виявлено вірогідну різницю (у сім’ях хлопчиків з ММД показники вірогідно вищі) (р < 0,05). У рубриках «Емоційне функціонування», «Фізичне функціонування» та «Соціальне функціонування» цього ж опитувальника середні значення в родинах хлопчиків із ЗПМР були вірогідно вищими, ніж у сім’ях хлопчиків зі СДУГ (р < 0,01).
В рубриці «Розумове функціонування» середні значення у сім’ях дівчаток із ЗПМР були вірогідно вищими, ніж у батьків дівчаток із РАС (р < 0,01). У рубриці «Відносини в родині» показники родин хлопчиків зі СДУГ були вірогідно вищими, ніж у сімей дівчаток із цим же психомоторним порушенням (р < 0,05). У цій же рубриці середні показники сімей хлопчиків зі СДУГ вірогідно перевищували показники родин хлопчиків із ЗПМР (р < 0,01). У рубриці «Підсумковий бал функціонування родини» (The Family Functioning Summary Score) показники родин хлопчиків із ЗПМР були вірогідно вищими, ніж у сім’ях дівчаток (р < 0,01).
У рубриці «Залучення сім’ї» опитувальника Healthcare Satisfaction Generic Module показники родин дівчаток зі СДУГ вірогідно перевищували показники батьків хлопчиків (р < 0,05). В цій же рубриці показники родин хлопчиків із ЗПМР вірогідно перевищували показники сімей хлопчиків з ММД (р < 0,05). Показники родин хлопчиків із ЗПМР цієї ж рубрики були вірогідно вищими, ніж у сімей хлопчиків зі СДУГ (р < 0,01). В сім’ях хлопчиків із РАС у даній рубриці показники вірогідно вищі, ніж у родинах хлопчиків зі СДУГ (р < 0,05).
Родини дівчаток зі СДУГ у рубриці «Комунікація» мали вірогідно вищі показники, ніж родини хлопчиків з цією ж неврологічною проблемою (р < 0,05). В сім’ях хлопчиків із ЗПМР та РАС верифікувалися вірогідно вищі показники, ніж у сім’ях хлопчиків зі СДУГ в цій же рубриці (р < 0,05 та р < 0,01 відповідно).
В рубриці «Технічні навички» середні показники в родинах хлопчиків зі СДУГ вірогідно перевищували показники сімей дівчаток з цим же психомоторним порушенням (р < 0,05). У цій же рубриці сім’ї хлопчиків із ЗПМР за своїми показниками вірогідно переважають показники, отримані у родинах хлопчиків зі СДУГ (р < 0,01). В рубриці «Загальне задоволення» родини хлопчиків із ЗПМР вірогідно перевершують сім’ї своїх однолітків зі СДУГ за своїми бальними показниками (р < 0,01).
У рубриці «Емоційне функціонування» опитувальника PedsQLTM 4.0 Generic Score Scales середні показники хлопчиків із ММД були вірогідно вищими, ніж у хлопчиків із ЗПМР (р < 0,05). В рубриці «Соціальне функціонування» цього ж опитувальника при порівнянні показників хлопчиків із ЗПМР, ММД та СДУГ виявлено, що показники хлопчиків з ММД вірогідно перевищували показники хлопчиків зі ЗПМР (р < 0,01), тоді як хлопчики із ЗПМР вірогідно переважали пацієнтів зі СДУГ (р < 0,01).
Середні показники хлопчиків з ММД в рубриці «Соціальне функціонування» вірогідно перевищували показники хлопчиків із РАС та СДУГ (відповідно р < 0,05, р < 0,01). Показники хлопчиків з ММД в рубриці «Функціонування у школі/дитсадку» вірогідно вищі, ніж показники хлопчиків із ЗПМР (р < 0,01). Показники хлопчиків із СДУГ цієї ж рубрики вірогідно перевищують показники хлопчиків із ЗПМР (р < 0,05).
В рубриці «Підсумковий бал психосоціального здоров’я» (Psychosocial Health Summary Score) відзначено вірогідне перевищення показників хлопчиків із ММД над пацієнтами із ЗПМР (р < 0,05).
Середні показники хлопчиків зі СДУГ в рубриці «Загальний бал» (Total score) опитувальника PedsQLTM 4.0 Generic Score Scales вірогідно перевищували показники хлопчиків із ЗПМР в даній рубриці (р < 0,05).
Середні показники хлопчиків зі СДУГ рубрики «Загальний бал» (Total score) опитувальника PedsQLTM 4.0 Generic Score Scales були вірогідно вищими за показники родин хлопчиків зі СДУГ у цій же рубриці опитувальника PedsQLTM Healthcare Satisfaction Generic Module (р < 0,01).
Середні показники сімей хлопчиків із ЗПМР рубрики «Загальний бал» (Total score) опитувальника PedsQLTM Healthcare Satisfaction Generic Module вірогідно перевищують показники родин дівчаток із цією ж нозологією у даній рубриці (р < 0,05).
Показники всіх обстежених хлопчиків в рубриці «Загальний бал» (Total score) опитувальника PedsQLTM 4.0 Generic Score Scales вірогідно перевищували показники родин хлопчиків у цій же рубриці опитувальника PedsQLTM Healthcare Satisfaction Generic Module (р < 0,05). Вірогідної різниці між показниками в інших рубриках виявлено не було.
Обговорення
Матері хлопчиків і дівчаток із порушеннями психомоторного розвитку, доглядаючи за дітьми, стикалися із дещо відмінними труднощами. Результати нашого дослідження встановили вірогідний зв’язок між наявними у хлопчиків психомоторними порушеннями (на прикладі всіх обстежених хлопчиків та хлопчиків із ЗПМР зокрема) та емоційним станом їхніх родин, що проявлялося схильністю до тривожних розладів, відчуттям суму, невдачі, безнадії та безпорадності, що корелює із даними багатьох зарубіжних авторів [31–33]. Пригнічений емоційний стан матерів, які здійснюють щоденний догляд за дітьми, негативно позначався на їх соматичному стані. Зокрема, матері хлопчиків заявляли про постійне відчуття втоми (в тому числі вранці після прокидання), головний біль, які порушували їх стан, заважаючи займатися щоденними справами, труднощі із концентрацією та утриманням уваги, запам’ятовуванням інформації, прийняттям рішень в умовах дефіциту часу, постійне занепокоєння станом здоров’я дітей, ефективністю діагностичних та лікувальних втручань, які щодо них здійснюються, острах щодо реакції з боку інших на стан дитини та стурбованість його впливом на ситуацію в родині (особливо у родинах хлопчиків із ЗПМР), часте виникнення у ній конфліктів, брак спілкування, напруженість у стосунках між її членами, складнощі у спільному прийнятті рішень ними; матері дівчаток у той же час були більше занепокоєні відчуттям ізольованості від інших членів сім’ї, браком підтримки з їх боку. Разом із тим відсутність розуміння ситуації в родинах з боку оточуючих, складнощі у комунікації з ними (в тому числі з медпрацівниками), відчуття постійної, дедалі вираженішої втоми, яка значно утруднювала виконання хатньої роботи, поглинаючи все більше часу та зусиль, були факторами, із якими стикалися матері дітей обох статей.
У нашому дослідженні у родинах хлопчиків (особливо в родинах хлопчиків із ЗПМР) верифіковано вірогідну зворотну залежність між HRQOL (інтегрального показника, що включає психічні, фізичні та соціальні фактори) та наявною неврологічною патологією, що узгоджується із результатами інших досліджень [2].
Матері як хлопчиків (особливо із ЗПМР та РАС), так і дівчаток при контактах із системою охорони здоров’я надають великого значення обсягу інформації про стан здоров’я дітей та його динаміку, встановлений їм діагноз, необхідні медичні втручання та їх результати; провідну роль для них відіграють комунікативні навички медпрацівників, їх чуйність до потреб дитини, вміння вислухати, роз’яснити всі аспекти медичних втручань, їхня здатність враховувати емоційні потреби дітей (зокрема, із ЗПМР). При цьому матері хлопчиків більшу увагу звертали на чуйність медперсоналу, його готовність надати повну інформацію про стан дитини, залучити батьків до догляду за нею та обговорювати з ними всі його аспекти, а також відповісти на запитання, що стосуються стану здоров’я дітей.
Також, за даними анкетування батьків щодо якості життя дітей, в обстежених хлопчиків (вірогідна кореляція із ЗПМР) верифіковано вірогідний вплив наявних у них психомоторних порушень на такі інтегральні складові показника якості життя, як фізичне, емоційне та соціальне функціонування (участь у спортивних активностях, виконання доручень, наявність сформованих навичок самообслуговування, порушень сну, відчуття страху, суму, занепокоєння, вміння налагоджувати стосунки з іншими дітьми (як в дитячому колективі, так і поза ним)). Наявність того чи іншого неврологічного порушення, як свідчать результати нашого дослідження, як у хлопчиків (вірогідна кореляція із ЗПМР), так і в дівчаток вірогідно пов’язана з успішністю в навчанні, кількістю пропущених днів через хворобу чи необхідністю візиту до лікаря, здатністю концентрувати та утримувати увагу під час занять.
Отже, надзвичайно важливою є підтримка родин дітей із психомоторними порушеннями із боку як найближчого оточення, так і держави шляхом застосування додаткових соціальних програм, залучення батьків до різноманітних груп підтримки за участю психологів із метою розробки адекватних стратегій подолання та корекційних програм, спрямованих на реабілітацію членів родин цієї категорії дітей. З огляду на складні соціально-економічні умови, гострим залишається питання якості і доступності медичних послуг для цієї групи дітей та їх родин, зокрема, через скорочення мережі медичних закладів, що є особливо актуальним для сільської місцевості [78–81].
Висновки
1. Установлено наявність прямого вірогідного кореляційного зв’язку різної сили між середніми показниками обстежених хлопчиків із порушеннями психомоторного розвитку, хлопчиків із ЗПМР, а також їхніх родин із наявною в дітей неврологічною патологією. Кореляційний зв’язок між показниками дівчаток та їхніх родин, а також наявними в них неврологічними розладами у більшості рубрик був невірогідним.
2. Зворотну вірогідну кореляцію різної сили виявлено між показниками The Parent HRQL Summary Score опитувальника PedsQLTM 2.0 Family impact module, загальними показниками (Total score) опитувальника PedsQLTM Healthcare Satisfaction Generic Module, показниками Psychosocial Health Summary та загальними показниками (Total score) опитувальника PedsQLTM 4.0 Generic Score Scales всіх обстежених хлопчиків (та хлопчиків із ЗПМР), а також їхніх родин та неврологічними порушеннями у дітей.
3. Внаслідок проведеного аналізу результатів анкетування верифіковано наявність вірогідно вищих (за незначним винятком) середніх показників хлопчиків та їхніх родин з порушеннями психомоторного розвитку порівняно з дівчатками та їхніми сім’ями в деяких рубриках всіх використовуваних опитувальників. Показники дітей із ЗПМР та їхніх родин (переважно хлопчиків) у більшості випадків вірогідно перевищували значення в дітей з іншими неврологічними порушеннями та у їхніх родин.
4. Вірогідної кореляції в решти дітей та їхніх родин, а також вірогідної різниці між іншими показниками не виявлено. При цьому між показниками хлопчиків зі СДУГ та наявною у них неврологічною нозологією не виявлено кореляційного зв’язку.
5. Вважаємо за доцільне проведення подальших досліджень із залученням більшого числа учасників для підвищення вірогідності отриманих даних.
Конфлікт інтересів. Автори заявляють про відсутність конфлікту інтересів та власної фінансової зацікавленості при підготовці даної статті.
Інформація про внесок кожного автора. Няньковський С.Л. — концепція і дизайн дослідження, редагування тексту статті; Пишник А.І. — збирання й обробка матеріалів, аналіз отриманих даних, написання тексту.
Отримано/Received 11.03.2022
Рецензовано/Revised 23.03.2022
Прийнято до друку/Аccepted 04.04.2022
Список литературы
1. Misura A.K., Memisevic H. Quality of life of parents of children with intellectual disabilities in Croatia. Journal of educational and social research. 2017. № 7(2). P. 43-48. doi: 10.5901/jesr.2017.v7n2p43.
2. Lemmon M.E., Huffstetler H.E., Reeve B.B. Measuring health-related quality of life in pediatric neurology. J. Child Neurol. 2020. № 35(10). P. 681-689. doi: 10.1177/0883073820923809. PMID: 32498657. PMCID: PMC7415579.
3. Marker A.M., Steele R.G., Noser A.E. Physical activity and health-related quality of life in children and adolescents: a systematic review and meta-analysis. Health Psychol. 2018. № 37(10). P. 893-903. doi: 10.1037/hea0000653. PMID: 30234348.
4. Koвтюк Н.І. Аналіз оцінки показників якості життя у дітей. Буковинський медичний вісник. 2012. Т. 16. № 4(64). С. 195-200.
5. Fridman M., Banaschewski T., Sikirica V., Quintero J., Erder H.M., Chen K.S. Caregiver perspective on pediatric attention-deficit/hyperactivity disorder: medication satisfaction and symptom control. Neuropsychiatr. Dis. Treat. 2017. № 13. P. 443-455. doi: 10.2147/NDT.S121639. PMCID: PMC5315351. PMID: 28243096.
6. Ketelaar M., Bogossian A., Saini M., Meily-Visser A., Lach L. Assessment of the family environment in pediatric neurodisability: a state-of-the-art review. Dev. Med. Child Neurol. 2017. № 59(3). P. 259-269. doi: 10.1111/dmcn.13287 PMID: 27696390.
7. Dykens E.M. Family adjustment and interventions in neurodevelopmental disorders. Curr. Opin. Psychiatry. 2015. № 28(2). P. 121-126. doi: 10.1097/YCO.0000000000000129. PMCID: PMC5348480. PMID: 25594421.
8. Шлюз Б. Дитина з ускладненою інвалідністю в сім’ї. Дослідження випадку. Вісник Львівського університету. Серія педагогічна. 2016. № 31. С. 362-370.
9. Lamsal R., Ungar W.J. Impact of growing up with a sibling with a neurodevelopmental disorder on the quality of life of an unaffected sibling: a scoping review. Disability and rehabilitation. 2021. № 43(4). P. 586-594. doi: 10.1080/09638288.2019.1615563.
10. Schertz M., Karni-Visel Y., Tamir A., Genizi J., Roth D. Family quality of life among families with a child who has a severe neurodevelopmental disability: impact of family and child socio-demographic factors. Reserarch in developmental disabilities. 2016. № 53-54. P. 95-106. doi.org/10.1016/j.ridd.2015.11.028.
11. Kachooei H., Daneshmand R., Dolatshahi B., Samadi R., Samiei M. Attention-deficit/hyperactivity disorder and martial satisfaction: the preliminary roles of employment and income. Iran J. Psychiatry Behav. Sci. 2016. № 10(2). P. e4012. doi: 10.17795/ijpbs-4012. PMCID: PMC5088356. PMID: 27803722.
12. Larsen Moen Ø. Everyday life in families with a child with ADHD and public health nurses’ conceptions of their role. Karlstadt: Universitetstryckeriet, 2014. P. 1-68.
13. Fairfax A., Brehaut J., Colman I. et al. A systematic review of the association between coping strategies and quality of life among caregivers of children with chronic illness and/or disability. BMC Pediatrics. 2019. № 19(1). P. 215. doi: 10.1186/s12887-019-1587-3.
14. Da Paz N.S., Siegel B., Coccia M.A., Epel E.S. Acceptance or despair? Maternal adjustment to having a child diagnosed with autism. J. Autism Dev. Disord. 2018. № 48(6). P. 1971-1981. doi: 10.1007/s10803-017-3450-4. PMID: 29307036. PMCID: PMC6347022.
15. Johnsson U., Alaie I., Loefgren W.A. et al. Annual research review: quality of life and childhood mental and behavioural disorders — a critical review of the research. J. Child Psychol. Psychiatry. 2017. № 58(4). P. 439-469. doi: 10.1111/jcpp.12645. PMID: 27709604.
16. Sheng N., Ma J., Ding W., Zhang Y. Effects of caregiver-involved interventions on the quality of life of children and adolescents with chronic conditions and their caregivers: a systematic review and meta-analysis. Qual. Life Res. 2019. № 28(1). P. 13-33. doi: 10.1007/s11136-018-1976-3. PMID: 30167936.
17. Adib N.A.N., Ibrahim M.I., Ab Rahman A. et al. Predictors of caregivers’ satisfaction with the management of children with autism spectrum disorder: a study at multiple levels of health care. Int. J. Environ. Res. Public Health. 2019. № 16(10). P. 1684. doi: 10.3390/ijerph16101684. PMID: 31091735. PMCID: PMC6572543.
18. Vernhet C., Dellepiazza F., Blanc N. et al. Coping strategies of parents of children with autism spectrum disorder: a systematic review. Eur. Child Adolesc Psychiatry. 2019. № 28(6). P. 747-758. doi: 10.1007/s00787-018-1183-3. PMID: 29915911.
19. Ganjiwale D., Ganjiwale J., Sharma B., Mishra B. Quality of life and coping strategies of caregivers of children with physical and mental disabilities. J. Family Med. Prim. Care. 2016. № 5(2). P. 343-348. doi: 10.4103/2249-4863.192360. PMCID: PMC5084559. PMID: 27843839.
20. Goodson A., Juniper T., Lloyd C., Miller H., Reid P., Rose M. Audit of the quality of medical reports for children with special educational needs. Archives of disease in childhood. 2015. № 100. P. A196-A197. doi: 10.1136/archdischild-2015-308599.421.
21. Марценковський І.А., Марценковська І.І. Розлади аутистичного спектра: фактори ризику, особливості діагностики й терапії. Міжнародний неврологічний журнал. 2018. № 4(98). С. 75-83. doi: 10.22141/2224-0713.4.98.2018.139429.
22. Ruble L., Murray D., McGrew J.H., Brevoort K., Wong V.W. A preliminary study of activation, stress, and self-management of parents of children with autism spectrum disorder. J. Child Fam. Stud. 2018. № 27. P. 825-834. doi: 10.1007/s10826-017-0814-5.
23. Hutchinson L., Feder M., Abar B., Winsler A. Relations between parenting stress, parenting style, and child executive functioning for children with ADHD or autism. Journal of Child and Family Studies. 2016. № 25. P. 3644-3656. doi: 10.1007/s10826-016-0518-2.
24. Factor R.S., Swain D.M., Scarpa A. Child autism spectrum disorder traits and parenting stress: the utility of using a physiological measure of parental stress. J. Autism Dev. Disord. 2018. № 48(4). P. 1081-1091. doi: 10.1007/s10803-017-3397-5. PMID: 29164443.
25. Bozkurt G., Uysal G., Düzkaya D.S.Examination of care burden and stress coping styles of parents of children with autism spectrum disorder. Journal of pediatric nursing. 2019. № 47. P. 142-147. doi: 10.1016/j.pedn.2019.05.005.
26. Hsiao Y.-J., Higgins K., Pierce T., Schaeffer Whitby P.J., Tandy R.D. Parental stress, family quality of life, and family-teacher partnerships: Families of children with autism spectrum disorder. Research in developmental disabilities. 2017. № 70. P. 152-162. doi: 10.1016/j.ridd.2017.08.013.
27. Mathew N.E., Burton K.L.O., Schierbeek A., Crucec R., Walter A., Eapen V. Parenting preschoolers with autism:socioeconomic influences on wellbeing and sense of competence. World J. Psychiatry. 2019. № 9(2). P. 30-46. doi: 10.5498/wjp.v9.i2.30. PMCID: PMC6422881. PMID: 30915270.
28. Wang Y., Xiao L., Chen R.-S. et al. Social impairment of children with autism spectrum disorder affects parental quality of life in different ways. Psychiatry Res. 2018. № 266. P. 168-174. doi: 10.1016/j.psychres.2018.05.057. PMID: 29864617.
29. Manan A.I.A., Amit N., Said Z., Ahmad M. The influences of parenting stress, children behavioral problems and children quality of life on depression symptoms among parents of children with autism: preliminary findings. Jurnal Sains Kesihatan Malaysia. 2018. P. 137-143. doi: 10.17576/JSKM-2018-19.
30. Стукан Л.В.Особливості ставлення матері до дитини з аутистичними розладами. Український вісник психоневрології. 2014. Т. 22. № 2(79). С. 124-127.
31. Kousha M., Attar A.H., Shoar Z. Anxiety, depression, and quality of life in Iranian mothers of children with autism spectrum disorder. J. Child Health Care. 2016. № 20(3). P. 405-414. doi: 10.1177/1367493515598644. PMID: 26311483.
32. Fernandez-Alcantara M., Garcia-Caro M.P., Perez-Marfil M.N., Hueso-Montoro C., Laynez-Rubio C., Cruz-Quintana F. Feelings of loss and grief in parents of children diagnosed with autism spectrum disorders (ASD). Res. Dev. Disabil. 2016. № 55. P. 312-321. doi: 10.1016/j.ridd.2016.05.007. PMID: 27235768.
33. Foody C., James J.E., Leader G. Parenting stress, salivary biomarkers and ambulatory blood pressure: a comparison between mothers and fathers of children with autism spectrum disorders. J. Autism Dev. Disord. 2015. № 45 (4). P. 1084-1095. doi: 10.1007/s10803-014-2263-y. PMID: 25287900.
34. Adams D., Clark M., Simpson K. The relationship between child anxiety and the quality of life of children and parents of children on the autism spectrum. J. Autism Dev. Disord. 2020. № 50(5). P. 1756-1769. doi: 10.1007/s10803-019-03932-2. PMID: 30805767.
35. McAuliffe T., Cordier R., Vaz S., Thomas Y., Falkmer T. Quality of life, coping styles, stress levels, and time use in mothers of children with autism spectrum disorders: comparing single versus coupled households. J. Autism Dev. Disord. 2017. № 47(10). P. 3189-3203. doi: 10.1007/s10803-017-3240-z. PMID: 28730416.
36. Craig F., Operto F.F., De Giacomo A.et al. Parenting stress among parents of children with neurodevelopmental disorders. Psychiatry Res. 2016. № 242. P. 121-129. doi: 10.1016/j.psychres.2016.05.016. PMID: 27280521.
37. McGrew J.H., Keyes M.L. Caregiver stress during the first year after diagnosis of an autism spectrum disorder. Research in autism spectrum disorders. 2014. № 8(10). P. 1373-1385. doi: 10.1016/j.rasd.2014.07.011.
38. Baylot L., Zanksas S., Meindl J.N., Parra G.R., Cogdal P., Powell K. Parental symptoms of posttraumatic stress following a child’s diagnosis of autism spectrum disorder: A pilot study. Research in autism spectrum disorders. 2012. № 6(3). P. 1186-1193. doi: 10.1016/j.rasd.2012.03.008.
39. Ten Hoopen L.W., De Nijs P.F.A., Duvekot J. et al. Children with an autism spectrum disorder and their caregivers: capturing health-related and care-related quality of life. J. Autism Dev. Disord. 2020. № 50(1). P. 263-277. doi: 10.1007/s10803-019-04249-w. PMID: 31625009. PMCID: PMC6946729.
40. Burrell A., Ives J., Unwin G. The experiences of fathers who have offspring with autism spectrum disorder. J. Autism Dev. Disord. 2017. № 47(4). P. 1135-1147. doi: 10.1007/s10803-017-3035-2. PMID: 28132126. PMCID: PMC5357286.
41. Muratori F., Turi M., Prosperi M. et al. Parental perspectives on psychiatric comorbidity in preschoolers with autism spectrum disorders receiving publicly funded mental health services. Front Psychiatry. 2019. № 10. P. 107. doi: 10.3389/fpsyt.2019.00107. PMCID: PMC6422880. PMID: 30914976.
42. Kilincaslan A., Kocas S., Bozkurt S., Kaya I., Derin S., Aydin R. Daily living skills in children with autism spectrum disorder and intellectual disability: A comparative study from Turkey. Res. Dev. Disabil. 2019. № 85. P. 187-196. doi: 10.1016/j.ridd.2018.12.005. PMID: 30576945.
43. Пакулова-Троцька Ю.В., Няньковський С.Л. Проблеми соматичної патології у дітей з розладами аутистичного спектра. Здоровье ребенка. 2016. № 1(69). С. 63-67.
44. Niemczyk J., Fischer R., Wagner C., Burau A., Link T., von Gontard A. Detailed assessment of incontinence, psychological problems and parental stress in children with autism spectrum disorder. J. Autism Dev. Disord. 2019. № 49(5). P. 1966-1975. doi: 10.1007/s10803-019-03885-6. PMID: 30637526.
45. Kuhlthau K.A., McDonnell E., Coury D.L., Payakachat N., Macklin E. Associations of quality of life with health-related characteristics among children with autism. Autism. 2018. № 22(7). P. 804-813. doi: 10.1177/1362361317704420. PMID: 28691502.
46. Du R.Y., Yiu C.K.Y., King N.M. Health- and oral health-related quality of life among preschool children with autism spectrum disorders. Eur. Arch. Paediatr. Dent. 2020. № 21(3). P. 363-371. doi: 10.1007/s40368-019-00500-1. PMID: 31802429.
47. Leader G., Francis K., Mannion A., Chen J. Toileting problems in children and adolescents with parent-reported diagnoses of autism spectrum disorder. J. Dev. Phys. Disabil. 2018. № 30(2). P. 307-327. doi: 10.1007/s10882-018-9587-z.
48. Crowell J.A., Keluskar J., Gorecki A. Parenting behavior and the development of children with autism spectrum disorder. Comprehensive Psychiatry. 2019. № 90. P. 21-29. doi: 10.1016/j.comppsych.2018.11.007.
49. Hatta K., Hosozawa M., Tanako K., Shimizu T. Exploring traits of autism and their on functional disability in children with somatic symptom disorder. J. Autism Dev. Disord. 2019. № 49(2). P. 729-737. doi: 10.1007/s10803-018-3751-2. PMID: 30229361.
50. Hedgecock J.B., Dannemiller L.A., Shui A.M., Rapport M.J., Katz T. Associations of gross motor delay, behavior and quality of life in young children with autism spectrum disorder. Physther. 2018. № 98(4). P. 251-259. doi: 10.1093/ptj/pzy006.
51. Öztürk Ö., Erermis S., Ercan E.S. et al. Does the quality of life in autism spectrum disorder differ from other chronic disorders and healthy children. Anadolu Psikiyatri Dergisi. 2015. № 17(5). P. 1. doi: 10.5455/apd.185269.
52. Toscano C.V.A., Carvalho H.M., Ferreira J.P. Exercise effects for children with autism spectrum disorder: metabolic health, autistic traits and quality of life. Percept. Mot. Skills. 2018. № 125(1). P. 126-146. doi.org/10.1177/0031512517743823. PMID: 29226773.
53. Wolraich M., Hagan J., Allan C. et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2019. № 144 (4). P. e20192528. doi: 10.1542/peds.2019-2528.
54.Taylor H.G., Orchinik L., Fristad M.A. et al. Associations of attention deficit hyperactivity disorder (ADHD) at school entry with early academic progress in children born prematurely and fullterm controls. Learning and individual differences. 2019. № 69. P. 1-10. doi: 10.1016/j.lindif.2018.10.008.
55. Peasgood T., Bhardwaj A., Biggs K. et al. The impact of ADHD on the health and well-being of ADHD children and their siblings. Eur. Child Adolesc. Psychiatry. 2016. № 25(11). P. 1217-1231. doi: 10.1007/s00787-016-0841-6.
56. Kandemir H., Kiliç B.G., Ekinci S., Yüce M. An evaluation of the quality of life of children with ADHD and their families. Anadolu Psikiyatri Dergisi. 2014. № 15(3). P. 265-271. doi: 10.5455/apd.46202.
57. Banaschewski T., Coghill D., Zuddas A., editors. Oxford Textbook of Attention deficit hyperactivity disorder. New York: Oxford University Press, 2018. P. 453. doi: 10.1093/med/9780198739258.001.0001.
58. Lee Y., Yang H.-J., Chen V.C. et al. Meta-analysis of quality of life in children and adolescents with ADHD: By both parent proxy-report and child self-report using PedsQLTM. Research in Developmental Disabilities. 2016. № 51-52. P. 160-172. doi: 10.1016/j.ridd.2015.11.009.
59. Mulraney M., Giallo R., Sciberras E., Lycett K., Mensah F., Coghill D. ADHD symptoms and quality of life across a 12-month period in children with ADHD: alongitudinal study. Journal of Attention Disorders. 2017. № 23 (17). P. 1675-1685. doi: 10.1177/1087054717707046.
60. El-Monshed A.H., Fathy A.M., Shehata A.A.M. Association between sleep habits and quality of life in children with attention deficit hyperactivity disorder. American Journal of Nursing Research. 2020. № 8 (2). P. 297-302. doi: 10.12691/ajnr-8-2-20.
61. Schwörer M.C., Reinelt T., Petermann F., Petermann U.J. Influence of executive functions on the self-reported health-related quality of life of children with ADHD. Qual. Life Res. 2020. № 29. P. 1183-1192. doi: 10.1007/s11136-019-02394-4. PMID: 31900765.
62. Azazy S., Nour-Eldein H., Mikhail H., Ismail M. Quality of life and family function of parents of children with attention deficit hyperactivity disorder. Eastern Mediterranean health journal = La revue de santé de la Méditerranée orientale = al-Majallah al-ṣiḥḥīyah li-sharq al-mutawassiṭ. 2018. № 24(6). P. 579-587. doi: 10.26719/2018.24.6.579.
63. Craig F., Savino R., Fanizza I., Lucarelli E., Russo L., Trabacca A. A systematic review of coping strategies in parents of children with attention deficit hyperactivity disorder (ADHD). Rev. Des. Disabil. 2020. № 98. P. 103571. doi: 10.1016/j.ridd.2020.103571.
64. Galloway H., Newman E., Miller N., Yuill C. Does parent stress predict the quality of life of children with a diagnosis of ADHD? A comparison of parent and child perspectives. J. Atten. Disord. 2019. № 23 (5). P. 435-450. doi: 10.1177/1087054716647479.
65. Walls M., Cabral H., Feinberg E., Silverstein M. Association between changes in caregiver depressive symptoms and child Attention-Deficit/Hyperactivity Disorder symptoms. J. Dev. Behav. Pediatr. 2018. № 39(5). P. 387-394. doi: 10.1097/DBP.0000000000000562.
66. Malakar P., Ghosh S. Comparative analysis of stress, anxiety and depression between the parents of children with autism and ADHD. International Journal of Health Sciences & Research. 2018. № 8(6). P. 242-248.
67. Chang C.-C., Chen Y.-M., Liu T.-L., Hsiao R.C., Chou W.-J., Yen C.-F. Affiliate stigma and related factors in family caregivers of children with Attention-Deficit/Hyperactivity Disorder. Int. J. Environ. Res. Public Health. 2020. № 17 (2). P. 576. doi: 10.3390/ijerph17020576. PMCID: PMC7013698. PMID: 31963190.
68. Al Balushi N., Al Shukaili M., Al Adawi S. Burden for caregivers of children with Attention-deficit/Hyperactivity Disorder in Oman. European Psychiatry. 2017. № 41(S1). P. S120-S121. doi: 10.1016/j.eurpsy.2017.01.1914.
69. Mostafavi M., Areshtanab H.N., Ebrahimi H., Vahidi M., Amiri S., Norouzi S. Caregiver burden and related factors in Iranian mothers of children with attention-deficit hyperactivity disorder. Nursing and midwifery studies. 2020. № 9(3). P. 149-156. doi: 10.4103/nms.nms_83_19.
70. Park B.-E., Lee J.-S., Kim H.-Y. et al. The influence of depression and school life on the quality of life of Korean child and adolescent patients with Attention-Deficit/Hyperactivity Disorder:a comparison of the perspectives of the patients and their caregivers. Journal of the Korean Academy of Child and Adolescent Psychiatry. 2019. № 30 (1). P. 2-8. doi: 10.5765/jkacap.180027. PMCID: PMC7289493. PMID: 32595314.
71. Померанцева Т.І., Скоробагатова О.В. Характеристика клініко-нейропсихологічного поліморфізму дітей з затримкою психомовленнєвого розвитку. Сучасні підходи до діагностики та лікування захворювань нервової системи у дітей: мат-ли наук.-практ. конф. Український вісник психоневрології. (м. Харків, 19–20 вер. 2020 р.). Харків, 2020. Т. 27. № 3. С. 102.
72. Dovgan K.N., Mazurek M.O. Differential effects of child difficulties on family burdens across diagnostic groups. Journal of Child and Family Studies. 2018. № 27. P. 872-884. doi: 10.1007/s10826-017-0944-9.
73. Mishra K., Siddharth V. Factors influencing institutional-based pediatric rehabilitation services among caregivers of children with developmental delay in southwestern Rajasthan. J. Neurosci Rural. Pract. 2018. № 9(1). P. 36-41. doi: 10.4103/jnrp.jnrp_283_17. –PMCID: PMC5812157. PMID: 29456343.
74. Dennis M.L., Neece C.L., Fenning R.M. Investigating the influence of parenting stress on child behavior problems in children with developmental delay: the role of parent-child relational factors. Advances in Neurodevelopmental Disorders. 2018. № 2(6). P. 129-141. doi: 10.1007/s41252-017-0044-2.
75. Emerson E., Brigham P. Exposure of children with developmental delay to social determinants of poor health: cross-sectional case record review study. Child: Care, Health and Development. 2015. № 41(2). P. 249-257. doi: 10.1111/cch.12144.
76. Mugal S.A. The influence of the family on the development of psychosomatic disorders in preschool children with mental retardation. Psychology Research. 2016. № 6(5). P. 270-274. doi: 10.17265/2159-5542/2016.05.002.
77. Танцура Л.М., Пилипець О.Ю., Третьяков Д.В., Трембовецька О.В. Механізми формування, підходи до ранньої діагностики та корекції мінімальної мозкової дисфункції у дітей. Медичний форум. 2016. № 7 (07). С. 177-181.
78. Shakespeare T., Bright T., Kuper H. Access to health for persons with disabilities. Available from: https://www.ohchr.org/_layouts/15/WopiFrame.aspx?sourcedoc=/Documents/Issues/Disability/StandardHealth/BackgroundDoc_EGM_Righttohealth.docx&action=default&DefaultItemOpen=1. Accessed: June 12, 2021.
79. Laugensen B., Lauritsen M.B., Jorgensen R., Sorensen E.E., Gronkjær M., Rasmussen P. ADHD and everyday life: Healthcare as a significant lifeline. Journal of pediatric nursing. 2017. № 35. P. 105-112. doi: 10.1016/j.pedn.2017.03.001.
80. Vergunst R., Swartz L., Hem K.-M. et al. Access to health care for persons with disabilities in rural South Africa. BMC Health Services Research. 2017. № 17. P. 741. Doi: 10.1186/s12913-017-2674-5.
81. Горачук В.В. Медико-соціальне обгрунтування моделі системи управління якістю медичної допомоги: Дис... д-ра мед. наук: 14.02.03. Нац. мед. акад. післядиплом. освіти ім. П.Л. Шупика. Київ, 2015. 440 с.
82. Adhikary G., Shawon S.R., Ali W. et al. Factors influencing patients’ satisfaction at different levels of health facilities in Bangladesh: Results from patient exit interviews. PLoS One. 2018. № 13(5). P. e0196643. doi: 10.1371/journal.pone.0196643. PMCID: PMC5955531. PMID: 29768441.
83. Dizitzer Y., Meiri G., Flusser H., Michaelovski A., Dinstein I., Menashe I. Comorbidity and health services usage in children with autism spectrum disorder: a nested case-control study. Epidemiol. Psychiatr. Sci. 2020. № 29. P. e95. doi: 10.1017/S2045796020000050. PMID: 31987063. PMCID: PMC7214718.
84. Daniels A.M., Como A., Hergüner S., Kostadinova K., Stosic J., Shih A. Autism in southeast Europe: asurvey of caregivers of children with autism spectrum disorders. J. Autism Dev. Disord. 2017. 47(8). 2314-2325. doi: 10.1007/s10803-017-3145-x. PMID: 28480480.
85. Buescher A.V.S., Cidav Z., Knapp M., Mandell D.S. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014. № 168(8). P. 721-728. doi: 10.1001/jamapediatrics.2014.210.
86. Libutzki B., Ludwig S., May M., Jacobsen R.H., Reif A., Hartman C.A. Direct medical costs of ADHD and its comorbid conditions on basis of a claims data analysis. Eur. Psychiatry. 2019. № 58. P. 38-44. doi: 10.1016/j.eurpsy.2019.01.019. PMID: 30802682.
87. Adeosun I.I., Ogun O., Adegbohun A., Ijarogbe G., Fatiregun O. The burden on caregivers of children with attention-deficit hyperactivity disorder in Lagos Nigeria: prevalence and correlates. Journal of Education, Society and Behavioural Science. 2017. № 22(1). P. 1-7. doi: 10.9734/JESBS/2017/35582.
/9.jpg)
/10.jpg)