Список литературы
1. Sung H, Ferlay J, Siegel RL et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021/02/04; 2021; 71: 209-249. https://doi.org/10.3322/caac.21660.
2. Malvezzi M, Carioli G, Bertuccio P, Boffetta P, Levi F, La Vecchia C, Negri E. European cancer mortality predictions for the year 2018 with focus on colorectal cancer. Ann Oncol. 2018 Apr 1; 29(4): 1016-1022. doi: 10.1093/annonc/mdy033. PMID: 29562308.
3. Carmichael JC, Mills S. Anatomy and Embryology of the Colon, Rectum, and Anus. The ASCRS Textbook of Colon and Rectal Surgery, 2016. 3-26. doi: 10.1007/978-3-319-25970-3_1 (https://doi.org/10.1007/978-3-319-25970-3_1).
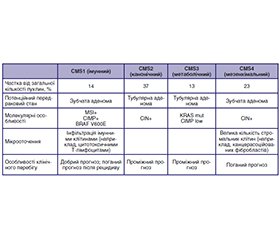
4. Guinney J, Dienstmann R, Wang X, de Reyniès A, Schli–cker A, Soneson C et al. The consensus molecular subtypes of colorectal cancer. Nature Medicine. 2015; 21(11): 1350-1356. doi: 10.1038/nm.3967 (https://doi.org/10.1038/nm.3967).
5. Puccini A, Marshall JL, Salem ME. Molecular Variances Between Right- and Left-sided Colon Cancers. Current Colorectal Cancer Reports. 2018. doi: 10.1007/s11888-018-0411-z (https://doi.org/10.1007/s11888-018-0411-z).
6. Brodsky FM. Pharmaceutical Research. 1988; 05(1): 1-9. doi: 10.1023/a:1015860525341 (https://doi.org/10.1023/a:1015860525341).
7. Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002; 347: 472-480. doi: 10.1056/NEJMoa020461.
8. Herbst R, Morgensztern D, Boshoff C. The biology and ma–nagement of non-small cell lung cancer. Nature. 2018; 553: 446-454. doi: 10.1038/nature2518.
9. Holderfield M, Deuker M, McCormick F, et al. Targeting RAF kinases for cancer therapy: BRAF-mutated melanoma and beyond. Nat Rev Cancer. 2014; 14: 455-467. doi: 10.1038/nrc3760.
10. Arteaga CL, Engelman JA. ERBB Receptors: From Oncogene Discovery to Basic Science to Mechanism-Based Cancer Therapeutics. Cancer Cell. 2014; 25(3): 282-303. doi: 10.1016/j.ccr.2014.02.025 (https://doi.org/10.1016/j.ccr.2014.02.025).
11. Tebbutt N, Pedersen MW, Johns TG. Targeting the ERBB family in cancer: couples therapy. Nature Reviews Cancer. 2013; 13(9): 663-673. doi: 10.1038/nrc3559 (https://doi.org/10.1038/nrc3559).
12. Normanno N, Tejpar S, Morgillo F, De Luca A, Van Cutsem E, Ciardiello F. Implications for KRAS status and EGFR-targeted therapies in metastatic CRC. Nat Rev Clin Oncol. 2009; 6: 519-527. doi: 10.1038/nrclinonc.2009.111.
13. Simanshu DK, Nissley DV, McCormick F. RAS proteins and their regulators in human disease. Cell. 2017; 170: 17-33. doi: 10.1016/j.cell.2017.06.009.
14. Dias Carvalho P, Guimaraes CF, Cardoso AP, et al. KRAS oncogenic signaling extends beyond cancer cells to orchestrate the microenvironment. Cancer Res. 2018; 78: 7-14. doi: 10.1158/0008-5472.CAN-17-2084.
15. Lievre A, Bachet JB, Le Corre D, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006; 66: 3992-3995. doi: 10.1158/0008-5472.CAN-06-0191.
16. Amado RG, Wolf M, Peeters M, et al. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol. 2008; 26: 1626-1634. doi: 10.1200/JCO.2007.14.7116.
17. Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F, et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res. 2007; 67: 2643-2648. doi: 10.1158/0008-5472.CAN-06-4158.
18. Karapetis CS, Khambata-Ford S, Jonker DJ, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008; 359: 1757-1765. doi: 10.1056/NEJMoa0804385.
19. Van Cutsem E, Lenz HJ, Kohne CH, et al. Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol. 2015; 33: 692-700. doi: 10.1200/JCO.2014.59.4812.
20. Ciardiello F, Normanno N, Maiello E, et al. Clinical acti–vity of FOLFIRI plus cetuximab according to extended gene mutation status by next-generation sequencing: findings from the CAPRI-GOIM trial. Ann Oncol. 2014; 25: 1756-1761. doi: 10.1093/annonc/mdu230.
21. Ros J, Baraibar I, Martini G, et al. The evolving role of consensus molecular subtypes: a step beyond inpatient selection for treatment of colorectal cancer. Curr Treat Options Oncol. 2021; 22: 113. doi: 10.1007/s11864-021-00913-5.
22. Irahara N, Baba Y, Nosho K, et al. NRAS mutations are rare in colorectal cancer. Diagn Mol Pathol. 2010; 19: 157-163. doi: 10.1097/PDM.0b013e3181c93fd1.
23. Nassar AH, Adib E, Kwiatkowski DJ. Distribution of KRASG12C somatic mutations across race, sex, and cancer type. N Engl J Med. 2021; 384: 185-187. doi: 10.1056/NEJMc2030638.
24. Schirripa M, Nappo F, Cremolini C, et al. KRAS G12C metastatic colorectal cancer: specific features of a new emerging target population. Clin Colorectal Cancer. 2020; 19: 219-225. doi: 10.1016/j.clcc.2020.04.009.
25. Tol J, Nagtegaal ID, Punt CJ. BRAF mutation in metastatic colorectal cancer [erratum in: N Engl J Med. 2011; 365: 869]. N Engl J Med. 2009; 361: 98-99. doi: 10.1056/NEJMc0904160.
26. Roth AD, Tejpar S, Delorenzi M, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol. 2010; 28: 466-474. doi: 10.1200/JCO.2009.23.3452.
27. Cohen R, Liu H, Fiskum J, et al. BRAF V600E mutation in first-line metastatic colorectal cancer: an analysis of individual patient data from the ARCAD database. J Natl Cancer Inst. 2021; 113: 1386-1395. doi: 10.1093/jnci/djab042.
28. Seppala TT, Bohm JP, Friman M, et al. Combination of microsatellite instability and BRAF mutation status for subtyping colorectal cancer. Br J Cancer. 2015; 112: 1966-1975. doi: 10.1038/bjc.2015.160.
29. Lochhead P, Kuchiba A, Imamura Y, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst. 2013; 105: 1151-1156. doi: 10.1093/jnci/djt173.
30. Fanelli GN, Dal Pozzo CA, Depetris I, et al. The heterogeneous clinical and pathological landscapes of metastatic Braf-mutated colorectal cancer. Cancer Cell Int. 2020; 20: 30. doi: 10.1186/s12935-020-1117-2.
31. Kopetz S, Grothey A, Yaeger R, et al. Encorafenib, binimetinib, and cetuximab in BRAF V600E-mutated colorectal cancer. N Engl J Med. 2019; 381: 1632-1643. doi: 10.1056/NEJMoa1908075.
32. Barras D, Missiaglia E, Wirapati P, et al. BRAF V600E mutant colorectal cancer subtypes based on gene expression. Clin Cancer Res. 2017; 23: 104-115. doi: 10.1158/1078-0432.CCR-16-0140.
33. Jones JC, Renfro LA, Al-Shamsi HO, et al. Non-V600 BRAF mutations define a clinically distinct molecular subtype of metastatic colorectal cancer. J Clin Oncol. 2017; 35: 2624-2630. doi: 10.1200/JCO.2016.71.4394.
34. Sepulveda AR, Hamilton SR, Allegra CJ, et al. Molecular biomarkers for the evaluation of colorectal cancer: guideline from the American Society for Clinical Pathology, College of American Pathologists, Association for Molecular Pathology, and the American Society of Clinical Oncology. J Clin Oncol. 2017; 35: 1453-1486. doi: 10.1200/JCO.2016.71.980.
35. Van Cutsem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016; 27: 1386-1422. doi: 10.1093/annonc/mdw235.
36. Mosele F, Remon J, Mateo J, et al. Recommendations for the use of next-generation sequencing (NGS) for patients with metastatic cancers: a report from the ESMO Precision Medicine Wor–king Group. Ann Oncol. 2020; 31: 1491-1505. doi: 10.1016/j.annonc.2020.07.014.
37. Russo A, Incorvaia L, Del Re M, et al. The molecular profi–ling of solid tumors by liquid biopsy: a position paper of the AIOM-SIAPEC-IAP-SIBioC-SIC-SIF Italian Scientific Societies. ESMO Open. 2021; 6: 100164. doi: 10.1016/j.esmoop.2021.100164.
38. Normanno N, Esposito Abate R, Lambiase M, et al. RAS testing of liquid biopsy correlates with the outcome of metastatic colorectal cancer patients treated with first-line FOLFIRI plus cetuximab in the CAPRI-GOIM trial. Ann Oncol. 2018; 29: 112-118. doi: 10.1093/annonc/mdx417.
39. Khan KH, Cunningham D, Werner B, et al. Longitudinal liquid biopsy and mathematical modeling of clonal evolution forecast time to treatment failure in the PROSPECT-C phase II colorectal cancer clinical trial. Cancer Discov. 2018; 8: 1270-1285. doi: 10.1158/2159-8290.CD-17-0891.
40. Patelli G, Vaghi C, Tosi F, et al. Liquid biopsy for prognosis and treatment in metastatic colorectal cancer: circulating tumor cells vs circulating tumor DNA [erratum in: Target Oncol. 2021; 16: 413]. Target Oncol. 2021; 16: 309-324. doi: 10.1007/s11523-021-00795-5.
41. Ross JS, Fakih M, Ali SM, et al. Targeting HER2 in colorectal cancer: the landscape of amplification and short variant mutations in ERBB2 and ERBB3. Cancer. 2018; 124: 1358-1373. doi: 10.1002/cncr.31125.
42. Bertotti A, Migliardi G, Galimi F, et al. A molecularly annotated platform of patient-derived xenografts (“xenopatients”) identifies HER2 as an effective therapeutic target in cetuximab-resistant colorectal cancer. Cancer Discov. 2011; 1: 508-523. doi: 10.1158/2159-8290.CD-11-0109.
43. Raghav K, Loree JM, Morris JS, et al. Validation of HER2 amplification as a predictive biomarker for anti-epidermal growth factor receptor antibody therapy in metastatic colorectal cancer. JCO Precis Oncol. 2019; 3: 1-13. doi: 10.1200/PO.18.00226.
44. Sartore-Bianchi A, Amatu A, Porcu L, et al. HER2 positivity predicts unresponsiveness to EGFR-targeted treatment in metastatic colorectal cancer. Oncologist. 2019; 24: 1395-1402. doi: 10.1634/theoncologist.2018-0785.
45. Pietrantonio F, Di Nicolantonio F, Schrock AB, et al. ALK, ROS1, and NTRK rearrangements in metastatic colorectal cancer. J Natl Cancer Inst. 2017; 109: djx089. doi: 10.1093/jnci/djx089.
46. Boland CR, Goel A. Microsatellite instability in colorectal cancer. Gastroenterology. 2010; 138: 2073-2087.e3. doi: 10.1053/j.gastro.2009.12.064.
47. Xiao Y, Freeman GJ. The microsatellite instable subset of colorectal cancer is a particularly good candidate for checkpoint blockade immunotherapy. Cancer Discov. 2015; 5: 16-18. doi: 10.1158/2159-8290.CD-14-1397.
48. Llosa NJ, Cruise M, Tam A, et al. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov. 2015; 5: 43-51. doi: 10.1158/2159-8290.CD-14-0863.
49. Ciardiello D, Vitiello PP, Cardone C, et al. Immunotherapy of colorectal cancer: challenges for therapeutic efficacy. Cancer Treat Rev. 2019; 76: 22-32. doi: 10.1016/j.ctrv.2019.04.003.