Резюме
Актуальність. Порушення функції руки є одним із факторів, що найбільш обмежують самообслуговування та виконання повсякденних дій пацієнтами із церебральним паралічем (ЦП). У дослідженнях останніх років продемонстровано ефективність інтенсивних багатокомпонентних методів реабілітації щодо покращення функції руки в дітей із ЦП. Одним iз таких методів є система інтенсивної нейрофізіологічної реабілітації, відома також як метод професора Козявкіна, — багатокомпонентна система, що поєднує різносторонні втручання в один інтенсивний курс. Метою цього дослідження було оцінити зміни функції руки в дітей із ЦП після двотижневого курсу реабілітації за методом Козявкіна. Матеріали та методи. У дослідженні брали участь 32 пацієнти віком 6–15 років зі спастичними формами ЦП (двостороннє ураження, I–III рівень за Системою класифікації функції руки). Усі пацієнти проходили двотижневий курс реабілітації за методом Козявкіна. Лікування тривало до 5 годин на день та складалося з фізичної терапії, ерготерапії, біомеханічної корекції хребта, рефлексотерапії, мобілізації суглобів, комп’ютерної ігротерапії та інших лікувальних впливів. Основним інструментом оцінки був тест функції руки Джебсена — Тейлора, а додатковими — опитувальник ABILHAND-kids, тест «Кубики в коробці» i динамометрія кисті. Результати. Статистично вірогідне покращення на 14,9 ± 38,0 секунди було виявлене при виконанні тесту Джебсена — Тейлора для домінантної руки. Зміни тесту «Кубики в коробці» також були статистично вірогідними та становили 2,0 ± 3,7 пункту для домінантної руки і 1,8 ± 2,8 пункту — для недомінантної. Сила руки не змінилася; підвищення оцінки за питальником ABILHAND-kids не було статистично вірогідним. Висновки. Після двотижневого курсу лікування за методом Козявкіна в дітей із церебральним паралічем покращилися функції руки, зокрема вправність обох рук та функціонування домінантної руки.
Актуальность. Нарушение функции руки является одним из факторов, которые больше всего ограничивают самообслуживание и выполнение повседневных действий пациентами с церебральным параличом (ЦП). В исследованиях последних лет продемонстрирована эффективность интенсивных многокомпонентных методов реабилитации для улучшения функции руки у детей с ЦП. Одним из таких методов является система интенсивной нейрофизиологической реабилитации, известная также как метод профессора Козявкина, — многокомпонентная система, объединяющая разносторонние вмешательства в один интенсивный курс. Целью этого исследования было оценить изменения функции руки у детей с ЦП после двухнедельного курса реабилитации по методу Козявкина. Материалы и методы. В исследовании принимали участие 32 пациента в возрасте 6–15 лет со спастическими формами ЦП (двустороннее поражение, I–III уровень по Системе классификации функции руки). Все пациенты проходили двухнедельный курс реабилитации по методу Козявкина. Лечение продолжалось до 5 часов в день и состояло из физической терапии, эрготерапии, биомеханической коррекции позвоночника, рефлексотерапии, мобилизации суставов, компьютерной игротерапии и других лечебных воздействий. Основным инструментом оценки был тест функции руки Джебсена — Тэйлора, а дополнительными — опросник ABILHAND-kids, тест «Кубики в коробке» и динамометрия кисти. Результаты. Статистически достоверное улучшение на 14,9 ± 38,0 секунды было обнаружено при выполнении теста Джебсена — Тэйлора для доминантной руки. Изменения теста «Кубики в коробке» также были статистически достоверными и составляли 2,0 ± 3,7 пункта для доминантной руки и 1,8 ± 2,8 пункта — для недоминантной. Сила руки не изменилась; увеличение оценки по опроснику ABILHAND-kids не было статистически достоверным. Выводы. После двухнедельного курса лечения по методу Козявкина у детей с церебральным параличом улучшились функции руки, в частности ловкость обеих рук и функционирование доминантной руки.
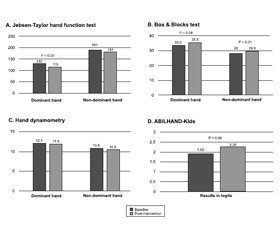
Background. Impaired hand function is one of the key factors that restrict the ability of patients with cerebral palsy (CP) to perform everyday activities and self-care. Recent studies show effectiveness of intensive multicomponent methods of rehabilitation for improving hand function in children with CP. One of such methods is Intensive Neurophysiological Rehabilitation System, also known as Professor Kozyavkin method, a multicomponent system that combines various interventions into one intensive course. The aim of this study was to assess changes in hand function in children with CP after the two-week rehabilitation course by Kozyavkin method. Materials and methods. Thirty-two patients with bilateral spastic CP (aged 6–15 years, Manual Ability Classification System level I–III) have participated in the study. All patients underwent the two-week rehabilitation course by Kozyavkin method. Treatment lasted up to 5 hours per day and included physical therapy, occupational therapy, spinal manipulative technique, reflexotherapy, joint mobilization, computer game therapy, and other interventions. The primary outcome measure was Jebsen-Taylor hand function test and the secondary outcome measures were ABILHAND-Kids questionnaire, Box and Blocks test, and hand dynamometry. Results. Statistically significant improvement by 14.9 ± 38.0 seconds was observed during Jebsen-Taylor test for the dominant hand. Changes in Box and Blocks test were also statistically significant and were equal to 2.0 ± 3.7 points for dominant hand and 1.8 ± 2.8 points for non-dominant hand. Grip strength did not change; increase in ABILHAND-Kids score was not statistically significant. Conclusions. Hand function, particularly dexterity of both hands and unimanual functions of the dominant hand, had improved in children with cerebral palsy after the two-week treatment course by Kozyavkin method.
Introduction
Hand function, the ability of the hands to perform properly in different contexts, is often restricted in children with cerebral palsy (CP) [1]. According to recent studies, 50–60 % of patients with CP suffer from upper limb impairments that considerably vary and include the fine motor deficit, decreased manual dexterity and weak grip strength [2–4]. Children with CP experience difficulties with pointing, reaching, grasping, manipulating, releasing and throwing objects. Consequently, children experience limitations in activities of daily life and participation restrictions [5].
There are many treatment programs aimed at improving hand function in children with CP [6–8]. Most promising results are shown in the studies of intensive, goal-oriented, high-dose, repetitive, incrementally challenging, functional interventions, such as a constraint-induced movement therapy and hand-arm bimanual intensive therapy [9, 10]. The common advantage of these interventions is the possibility to work through not only Body functions and Body structures domains but also Activity and Participation domains of the International Classification of Functioning, Disability and Health (ICF) [11]. So, the attention of both researchers and clinicians is focused on the exploration of intensive, goal- and function-oriented treatments addressing multiple limitations in children with CP.
One of such interventions is the Intensive Neurophysio-logical Rehabilitation System (INRS), also known as Kozyavkin method [12]. It combines different active and passive modalities within a two-week treatment course and is aimed at different functional goals within the ICF model [11]. The latest research demonstrated improvement in gross motor functions and a decrease of muscle spasticity in children with CP undergoing treatment with INRS [13, 14]. Improvement of the hand functions is also one of the most important targets of the INRS. Retrospective analysis of medical records of CP children reveals the improvement of fine motor function in 32 % of the whole group of patients [15].
Therefore, the aim of this pilot pre-post study is to assess changes of hand function in children with bilateral spastic cerebral palsy after the two-week intensive course using INRS.
Materials and methods
Study design
Single-arm, pre-post study design was used. Assessments were performed before and after a two-week treatment course by INRS, with patients serving as their own controls. The same evaluator assessed each child both times; evaluators were not involved in the study in another way. The study protocol was reviewed and approved by the local Ethical Commission of the International Rehabilitation Clinic (protocol number N-2018-02-12). Participants and their legal representatives received comprehensive information about the intervention and study design; written informed consent was obtained from legal representatives. Verbal consent was given by participants, when appropriate, based on age and cognitive skills. This pilot study was registered at clinicaltrials.gov with identifier NCT03454412.
Participants
All participants were patients of the International Rehabilitation Clinic. Eligibility criteria were: age 6 to 15 years, spastic forms of CP, bilateral impairment, level I–III according to the Manual Ability Classification System (MACS). Exclusion criteria were: severe epileptic syndrome, moderate to severe mental deficiency, inability to understand and comply with instructions, uncooperative behavior, severe contractures of upper extremity joints, and previous hand surgery. Forty-four patients were recruited. After applying the exclusion criteria, 32 patients were selected for the study. The demographic and clinical characteristics of the participants are presented in Table 1. The average age of the children was 10.2 years (SD = 2.9). Among them, 56.3 % were males, 56.3 % have a dominant right hand, 65.6 % were children with spastic quadriplegia, Gross Motor Function Classification System (GMFCS) level III was found in 40.6 % of patients, and MACS level II — in 46.8 %. The hand dominance in participants was established using the parental report and medical history.
/8.jpg)
Intervention
All patients underwent a two-week rehabilitation course by INRS, also known as the Professor Kozyavkin method. INRS is a novel multicomponent rehabilitation approach that combines versatile interventions into one intensive course [12]. The goal of INRS is to improve the functioning and quality of life of children with CP.
Treatment components are addressing different functional goals in the Body functions (joint mobility, muscle tone, voluntary movement, pain) and Activities and Participation (fine hand use, walking, moving around, interpersonal interactions and family relationships) domains of the ICF [11, 16]. The INRS course includes four to five hours of daily training, five days per week, for two weeks. Treatment is child-friendly and intensive at the same time. Interventions are aimed at improving different functions, influencing various pathogenic pathways and reaching the bigger total effect by potentiating each other. Treatment includes age-appropriate, goal-oriented tasks with consecutively increased difficulty. Unimanual and bimanual activities for training fine and gross motor functions are delivered in a child-friendly way with elements of play.
The individual treatment program is developed taking into account patient’s goals and condition, indications and contraindications. It may include the following components: physical therapy, occupational therapy, spinal manipulative technique, reflexotherapy, joint mobilization, computer game therapy, special massage system, strength training, physical exercises with movement correction suit, treadmill training for gait correction, vibration therapy, and group sessions of rhythmic gymnastics.
Physical therapy is performed daily and includes individualized exercises aimed at gross motor function training. It helps strengthen the muscles and improve the functional mobility of upper and lower extremities. Occupational the-rapy is focused on the development of skills necessary for the performance of everyday activities including play and self-care activities such as dressing, grooming and feeding, and fine motor tasks such as writing and drawing. The treatment program includes both unimanual and bimanual tasks. Full body massage incorporates classic, deep tissue, periosteal massage, trigger point therapy and muscle stretching techniques. Spinal manipulative therapy is used in a variation called “biomechanical correction of the spine”, in which the special high-velocity, low-amplitude thrusts techniques are used in lumbar, thoracic and cervical regions. Joint mobilization goals are to increase range of motion, decrease pain and improve the function of the extremities. During paraffin and wax applications, different muscle groups and joints are enveloped in warm paraffin and wax wraps. Reflexotherapy is a cutaneous electrical stimulation of acupuncture points with the use of the special low-current portable device. Strength training, or mechanotherapy, is aimed at building up muscle strength and endurance using various equipment and assistive technologies for resistance. Children play rehabilitation computer games, developed specifically for patients with movement disorders, using different game consoles and equipment (Nintendo Wii Fit with the balance board, Xbox with the Kinect motion sensor, Dance Mat) [17]. During movement correction suit therapy, physical exercises are performed using a special “Spiral” suit that provides extra loading on the trunk and extremities. It helps patients to correct movements and posture and attain new movement patterns [18]. Vibration therapy utilizes high-frequency, low-magnitude vibration to promote bone and muscle strength. Treadmill training is aimed at gait correction. Group session of rhythmic gymnastics includes dancing and performing exercises with the use of music in small groups of peers. A detailed description of the treatment system including indications and contraindications is presented in the rehabilitation manual of the Professor Kozyavkin method [12].
Outcome measures
The primary outcome measure was the Jebsen-Taylor hand function test (JTHFT). It evaluates fine and gross motor hand function using tasks that simulate activities of daily living [19]. The JTHFT consists of 7 items: writing a short sentence, turning over a card, picking up small common objects, simulated feeding using a teaspoon, stacking four checkers, moving large light cans and then large heavy cans. Administration guidelines specify that testing begins with the non-dominant hand. The writing task was excluded from the assessment due to the age of some children. Each item is scored according to the time taken to complete the task; time is rounded to the nearest second. The scores for all 6 items are then summed for a total score for each hand.
The secondary outcome measures were ABILHAND-Kids questionnaire, Box and Blocks test (BBT), and hand-grip dynamometry.
Manual dexterity is evaluated using BBT, a valid and reliable test [20]. The task is to carry wooden blocks from one compartment to another above the partition by one hand; only one block at a time is allowed to be transported. The score is the number of blocks carried in one minute.
Both JTHFT and BBT showed good reproducibility and responsiveness in children with CP. A recent study confirmed the reliability of the tests when the assessments were performed within two weeks and the responsiveness during intensive interventions [21].
ABILHAND-Kids is a measure of manual ability for children with upper limb impairments [22]. The parents were asked to fill in the Ukrainian version of the questionnaire by estimating their child’s performance of 20 unimanual and bimanual activities on a 3-level scale (impossible, difficult, easy) [23]. A total score is calculated and presented in the logits (the linear measure that expresses the odds of success of the patient in performing tasks) and the percentage of his/her performance.
Grip strength was quantified using Jamar hand dynamometer (Performance Health, USA). It displays results in kilograms. All children had three trials for each hand and the best result was saved.
Statistical analysis
Data analysis was performed using IBM SPSS v23 software. The normality of distribution was evaluated using the Kolmogorov-Smirnov test. Pre- and post-intervention values were compared using the paired sample t-tests.
Results
The parametric statistics was used to describe the data. Mean values at baseline and post-intervention assessment are summarized in Table 2 and Fig. 1.
Table 3 shows changes in the primary outcome measure — Jebsen-Taylor test and its subtests. An asterisk indicates a statistically significant difference where 2-tailed p-values are less than or equal to 0.05.
/10.jpg)
Jebsen-Taylor hand function test was the primary outcome measure in this study. Both hands were assessed separately. JTHFT total score for the dominant hand decreased by 14.9 seconds (SD = 38), from 130.1 to 115.2, after the treatment course using INRS in the whole group. The paired sample t-test showed that this change was statistically significant (p < 0.05). Non-dominant hand total score changed by 10.1 seconds; it was not significant (p > 0.05). We also compared the baseline and post-intervention values of JTHFT subtests. We observed statistically significant improvement in the results of lifting light objects by non-dominant hand (1.2, SD = 3.2, p < 0.05), simulated feeding by dominant hand (10, SD = 26.4, p < 0.05), lifting light objects by dominant hand (0.8, SD = 1.9, p < 0.05) and lifting heavy objects by dominant hand (1.9, SD = 2, p < 0.05).
Box and Blocks test was the secondary outcome measure aimed at assessing the dexterity of each hand separately. We noted meaningful changes in BBT results for both hands. For the dominant hand, the score improved by 2 blocks (SD 3.7, p < 0.05) and for non-dominant — by 1.8 blocks (SD 2.8, p < 0.001).
ABILHAND-Kids questionnaire also was a secondary outcome measure. The goal of this scale is to evaluate the hand function of the child in everyday life tasks. It includes both unimanual and bimanual tasks, they are not scored up separately, so this measure is not split by hands. ABILHAND-Kids score increased by 0.34 (0.98) logits, from 1.92 to 2.26, which was close to the statistically significant value (p = 0.06).
Hand dynamometry was the secondary outcome measure aimed at assessing the strength of hand grip. Changes of the grip strength of 0.24 kg for the dominant hand and 0.32 kg for non-dominant hand were not significant.
Discussion
The aim of this exploratory study was to assess the effect of the Kozyavkin method on hand function in children with cerebral palsy. We used JTHFT as a primary outcome measure and ABILHAND-Kids, BBT and hand-grip dynamometry as the secondary outcome measures.
We noted statistically significant improvements in the results of Jebsen-Taylor hand function test for dominant hand along with some of its components for both hands and Box and Blocks test for both hands.
JTHFT
The observed change of 14.9 seconds in total JTHFT score for the dominant hand was statistically significant. A decrease in JTHFT score means improvement of the hand function. To evaluate clinical significance of this change, we compared it with the smallest real difference (SRD) of 5.09 seconds for the total score of the dominant hand, measured in a sample of typically developed children [24]. The SRD is the smallest change in score between assessments that represents a true change over and above measurement error. We used the aforementioned SRD value for assessment since neither SRD for CP children nor minimal clinically important difference (MCID) is established for JTHFT. So, the detected difference of 14.9 seconds was greater than SRD. We can interpret this finding as clinically meaningful improvement of the dominant hand function after treatment by INRS.
We also observed statistically significant improvement in the results of the following JTHFT subtests: simulated feeding by dominant hand, lifting light objects by dominant hand, lifting heavy objects by dominant hand, and lifting light objects by non-dominant hand. A possible explanation of these findings may be that improved subtasks need similar types of movements and involvement of the same motor skills. Lifting and moving light and heavy large objects are actions that need more gross than fine motor skills and do not require precise fine manipulation to be completed. Simulated feeding is a task that needs a combination of the pincer grasp with gross manipulation but still can be accomplished without precise and coordinated use of fingers. These observations are in line with previous research concluding that treatment by INRS improves gross motor functions in children with CP [14].
Box and Blocks Test
We noted meaningful changes in BBT results for both hands: by 2 blocks per minute for dominant and by 1.8 blocks — for non-dominant. Higher BBT scores mean that manual dexterity has improved after the treatment. Since MCID is not established for BBT in children with CP, we have calculated it as a half of the standard deviation of the changes [25]. The result is considered clinically significant when the observed change is bigger than MCID. Improvements of both dominant and non-dominant hands were higher than calculated MCID values of 1.85 and 1.4, respectively. So, clinically meaningful improvement in manual dexterity of children with CP was noted after the course with INRS.
ABILHAND-Kids
ABILHAND-Kids improvement of 0.34 logits was close to statistically significant (p = 0.06). A possible explanation why positive changes didn’t reach significance level might be that the period between observations was short — only two weeks. Therefore, parents who filled in the questionnaire need some time to distinguish changes in their child’s abilities, and children need the time before they will start practice daily activities that were impossible or hard for them to accomplish earlier.
Hand dynamometry
We did not observe changes in grip strength after the treatment. But the study of other intensive rehabilitation techniques also did not show improvement of muscle strength while hand function and dexterity improved [26].
Our findings are in line with the result of the la-test research showed that intensive functional trainings can improve hand function in children with CP [27, 28]. Previous studies also showed that other high-intensity programs, combined of interventions for both upper and lower limbs and delivered during the short period of time, were effective for improving hand function in children with unilateral and bilateral spastic CP [29, 30].
INRS comprises all features that proved to be important for upper limb training to be successful — high intensity, relevance of training to daily life, the correspondence of training to the age and goals of the child [31]. One of the possible mechanisms of action of this short-term intense treatment is that interventions merged into the course with INRS are aimed at improving different functions, influencing various pathogenic pathways, and reaching the bigger total effect by potentiating each other.
Limitations
One of the limitations of our study is its short-term nature that makes it impossible to access long-term results. Another limitation is a lack of blinding due to the pre-post design with the absence of the control group. Another possible restraint is a relatively small sample size.
Currently, our team is conducting a double-blind randomized control trial with larger sample size and longer follow-up period to address all limitations of the present study and achieve more conclusive evidence. It was registered on clinicaltrials.gov under the identifier NCT04093180.
Conclusion
Hand function, particularly dexterity of both hands and unimanual functions of the dominant hand, had improved in children with cerebral palsy after the two-week treatment course by Kozyavkin method. Randomized controlled trials are needed for further investigation of this treatment system.
Acknowledgments
The authors want to thank all patients that give their consent to participate in the study as well as employees of International Rehabilitation Clinic for their help in conducting research.
Conflicts of interests. Authors declare the absence of any conflicts of interests and their own financial interest that might be construed to influence the results or interpretation of their manuscript.
Список литературы
1. Arnould C., Bleyenheuft Y., Thonnard J.L. Hand functioning in children with cerebral palsy. Frontiers in Neurology. 2014. 5. 48.
2. Yevtushenko S.K. Etiology and Pathogenesis of Cerebral Palsy in Children (A New Look at an Old Problem) (Lecture). International Neurological Journal. 2014. 3(65).
3. Arner M., Eliasson A., Nicklasson S., Sommerstein K., Hägglund G. Hand Function in Cerebral Palsy. Report of 367 Children in a Population-Based Longitudinal Health Care Program. The Journal of Hand Surgery. 2008. 33(8). 1337-1347.
4. Arnould C., Penta M., Thonnard J.L. Hand impairments and their relationship with manual ability in children with cerebral palsy. J. Rehabil. Med. 2007. 39(9). 708-14.
5. Klevberg G., Østensjø S., Krumlinde-Sundholm L., Elkjær S., Jahnsen R. Hand Function in a Population-Based Sample of Young Children with Unilateral or Bilateral Cerebral Palsy. Phys. Occup. Ther. Pediatr. 2017. 37(5). 528-540.
6. Novak I., Honan I. Effectiveness of paediatric occupational therapy for children with disabilities: а systematic review. Australian Occupational Therapy Journal. 2019 Apr 10.
7. Plasschaert V., Vriezekolk J., Aarts P., Geurts A., Van den Ende C. Interventions to improve upper limb function for children with bilateral cerebral palsy: a systematic review. Developmental Medicine & Child Neurology. 2019. 61(8). 899-907.
8. Shierk A., Lake A., Haas T. Review of Therapeutic Interventions for the Upper Limb Classified by Manual Ability in Children with Cerebral Palsy. Seminars in Plastic Surgery. 2016. 30(01). 14-23.
9. Gordon A.M., Schneider J.A., Chinnan A., Charles J.R. Efficacy of a hand-arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: а randomized control trial. Developmental Medicine & Child Neurology. 2007. 49(11). 830-838.
10. Hoare B.J., Wasiak J., Imms C., Carey L. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy. Cochrane Database Syst. Rev. 2007. (2). CD004149.
11. World Health Organization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization, 2001.
12. Kozyavkin V., Babadahly M., Lun H. et al. Intensive Neurophysiological Rehabilitation System — the Kozyavkin Method. A Manual for Rehabilitation Specialists. Lviv, Ukraine: Papuga Publishing House. 2012. 240 p.
13. Kachmar O., Mysula I., Kushnir A., Voloshyn T., Matiu-shenko O., Hasiuk M., Hordiyevych M. Changes in motor functions in children with cerebral palsy after the course of intensive neurophysiological rehabilitation: a single-blind study. International Neurological Journal. 2019. 5(107). 5-11.
14. Kachmar O., Voloshyn T., Hordiyevych M. Changes in muscle spasticity in patients with cerebral palsy after spinal manipulation: case series. Journal of Chiropractic Medicine. 2016. 15(4). 299-304.
15. Kozyavkin V.I., Kachmar O.O., Lysovych V.I. A retrospective analysis of the results of treatment with Intensive Neurophysiological Rehabilitation System. International Neurological Journal. 2018. 3(97). 14-20.
16. Schiariti V., Selb M., Cieza A., O’Donnell M. International Classification of Functioning, Disability and Health Core Sets for children and youth with cerebral palsy: a consensus meeting. Developmental Medicine & Child Neurology. 2015. 57(2). 149-158.
17. Kozyavkin V., Kachmar O., Markelov V., Melnychuk V., Kachmar B. Web-based Home Rehabilitation Gaming System for Balance Training. Journal of Accessibility and Design for All (CC). 2014. Special issue. 104-116.
18. Kozijavkin V., Kachmar O. Correction of Movement Utilizing the “Spiral” Suit — an Important Part of the Kozijavkin Method. Cerebral Palsy Magazine. 2004. 14-18.
19. Jebsen R., Taylor N., Trieschmann R., Trotter M., Howard L. An objective and standardized test of hand function. Archives of Physical Medicine and Rehabilitation. 1969. 50. 311-319.
20. Mathiowetz V., Volland G. et al. Adult norms for the Box and Block Test of manual dexterity. Am. J. Occup. Ther. 1985. 39(6). 386-391.
21. Araneda R., Ebner-Karestinos D., Paradis J., Saussez G., Friel K., Gordon A., Bleyenheuft Y. Reliability and responsiveness of the Jebsen-Taylor Test of Hand Function and the Box and Block Test for children with cerebral palsy. Developmental Medicine & Child Neurology. 2019. 61(10). 1182-1188.
22. Arnould C., Penta M., Renders A. et al. ABILHAND-Kids: A measure of manual ability in children with cerebral palsy. Neurology. 2004. 63(6). 1045-1052.
23. Hasiuk M., Arnould C., Kushnir A., Matiushenko O., Kachmar O. Cross-cultural adaptation and validation of the Ukrainian version of the ABILHAND-Kids questionnaire. Disability and Rehabilitation. 2019 Jun 19. 1-10.
24. Reedman S., Beagley S., Sakzewski L., Boyd R. The Jebsen Taylor Test of Hand Function: A Pilot Test-Retest Reliability Study in Typically Developing Children. Physical & Occupational Therapy in Pediatrics. 2015. 36(3). 292-304.
25. Norman G., Sloan J., Wyrwich K. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Medical Care. 2003. 41. 582-92.
26. Charles J., Wolf S., Schneider J., Gordon A. Efficacy of a child-friendly form of constraint-induced movement therapy in hemiplegic cerebral palsy: a randomized control trial. Developmental Medicine & Child Neurology. 2007. 48(8). 635-642.
27. Dong V., Tung I., Siu H., Fong K. Studies comparing the efficacy of constraint induced movement therapy and bimanual training in children with unilateral cerebral palsy: A systematic review. Developmental Neurorehabilitation. 2012. 16(2). 133-143.
28. Sakzewski L., Gordon A., Eliasson A. The State of the Evidence for Intensive Upper Limb Therapy Approaches for Children with Unilateral Cerebral Palsy. Journal of Child Neurology. 2014. 29(8). 1077-1090.
29. Saussez G., Brandão M., Gordon A., Bleyenheuft Y. Including a Lower-Extremity Component during Hand-Arm Bimanual Intensive Training does not Attenuate Improvements of the Upper Extremities: A Retrospective Study of Randomized Trials. Frontiers in Neurology. 2017. 8.
30. Bleyenheuft Y., Ebner-Karestinos D., Surana B., Paradis J., Sidiropoulos A., Renders A. et al. Intensive upper- and lower-extremity training for children with bilateral cerebral palsy: a quasi-randomized trial. Developmental Medicine & Child Neurology. 2017. 59(6). 625-633.
31. Reid L., Rose S., Boyd R. Rehabilitation and neuroplasticity in children with unilateral cerebral palsy. Nature Reviews Neurology. 2015. 11(7). 390-400.
/8.jpg)

/10.jpg)
/10_2.jpg)
/11.jpg)